Care Delivery Transformation Case Study: Dartmouth Health Connected Care Program
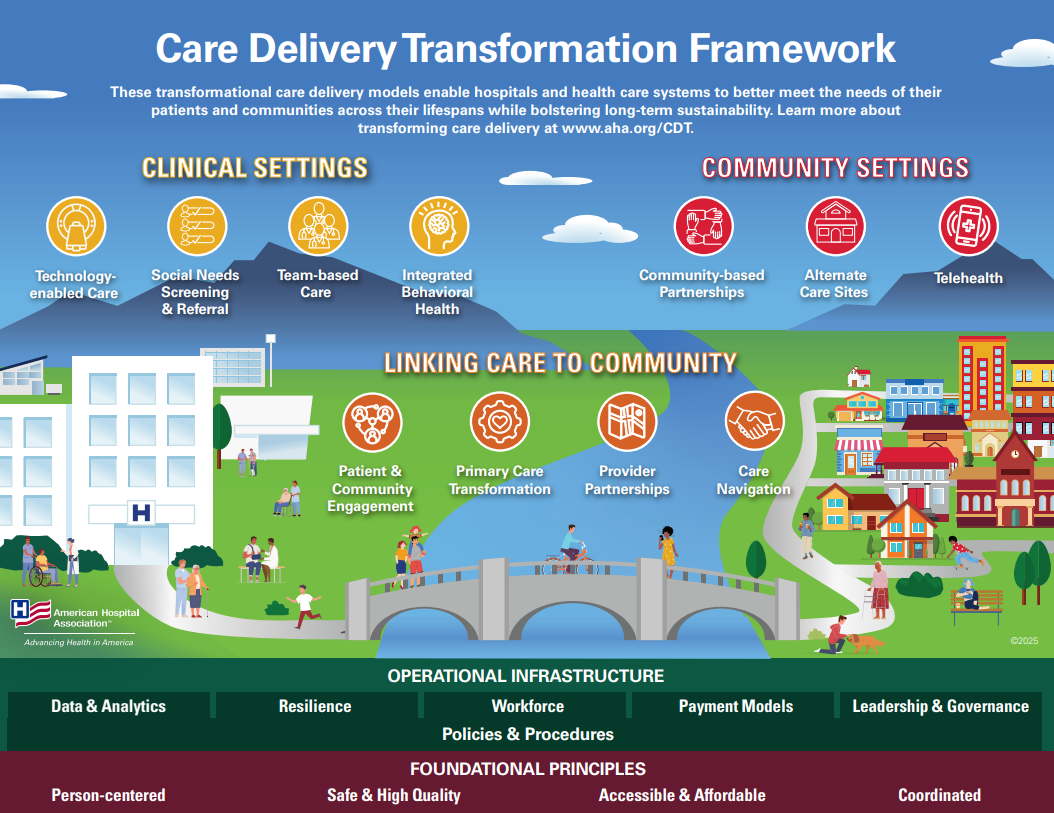
The Connected Care program leverages technology and partnerships to extend high-quality care in rural communities.
Background
Accessing medical care in rural America can be challenging due to several barriers. This is especially true in Northern New England — New Hampshire, Vermont and Maine, three of the most rural states in the U.S.
The region is characterized by mountainous terrain and remote communities scattered across wide distances. The population has large disparities in socioeconomic status and higher levels of chronic conditions than national averages. For many residents, the nearest hospital may be 90 minutes to three hours away, and specialty care is concentrated in the limited, more densely populated regions.
Dartmouth Health (DH) in New Hampshire and Vermont is working to extend medical care into rural communities through Connected Care, its Center for TeleHealth, designed to support rural clinicians as they provide specialty care to patients in their communities.
Approach
An early telehealth adopter, DH launched Connected Care in 2012 to increase access to specialty care throughout Northern New England, mitigate their medical center’s capacity constraints and address some foundational challenges of rural health and health care. The initiative was jumpstarted by a grant from the U.S. Department of Agriculture to support care in rural areas.
Partnering with rural hospitals throughout the region is at the heart of the program. DH clinicians utilize telehealth to support primarily rural hospitals with clinical expertise, helping patients receive high-quality care at their local facilities. Connected Care provides services to approximately 40 hospitals, many of which are critical access and most are outside the DH system.
Onboarding and relationship building is important to the process. Once a need is identified by a rural hospital that could potentially benefit from Connected Care’s support, the telehealth team begins working with a local project team to discuss services and the clinical needs of their patient population. Over the course of the implementation process, which can sometimes be accomplished in six weeks or less, Connected Care and local hospital teams spend time getting to know, understand and appreciate one another while also developing workflows and processes. Kevin Curtis, M.D., medical director of Connected Care, compared the partnership between his team and the rural hospitals as a true collaboration based on mutual respect as Connected Care clinicians work to become integral members of the outstanding bedside teams.
“We ask them, ‘How do we create a partnership with your department and your hospital and make the whole thing more efficient?’” said Matthew Maughan, Pharm.D., director of TelePharmacy. The DH team works to understand the culture, transportation, regional capacity and transfer patterns of the communities they serve so they can provide care recommendations that are aligned with the available resources.
A combination of three centralized hubs for some services, as well as remote clinicians in their office or dedicated private space at home for others, gives rural providers and patients access to psychiatrists, neurologists, emergency medicine physicians, intensivists, neonatologists, pharmacists, nurses and a host of other specialists.
When a patient arrives at a rural hospital in need of specialty care, local physicians in emergency departments, ICUs or other inpatient settings initiate the telehealth consultations which are then delivered via mobile carts, tablets or dedicated audiovisual equipment that is built right into the local hospital room. DH clinicians can communicate directly with the patient and the local provider, ensuring the patient receives the care they need in their local hospital.
Reach
Since its inception, Connected Care has participated in approximately:
- 38,000 TeleICU admissions.
- 26,000 TeleNeurology/Stroke consults.
- 3,800 TeleEmergency encounters.
- 4,500 emergency TelePsychiatry consults.
- 375 TeleICN (neonatologist) encounters.
- 6,000,000+ TelePharmacy orders.
Among the six 24/7 services listed above, Connected Care conducts approximately 50,000 video encounters and executes approximately 1 million TelePharmacy orders per year.
Connected Care also operates a central monitoring hub observing cardiac telemetry for more than 200 inpatient beds. The program also acts as a consultant for approximately 150,000 outpatient virtual visits per year within the DH system. Those scheduled outpatient virtual visits soared from 10 visits per day prior to the pandemic to over 2,000 visits per day during the peak period. DH now averages approximately 650 outpatient telehealth visits per day.
Outcomes
More important than the number of encounters is the impact; some examples are highlighted below.
- After an urgent/emergent TeleNeurology/Stroke consult, 93% of the patients complete their care at the local hospital and don’t require transfer.
- TeleEmergency avoided patient transfers in 13% of the cases.
- TelePsych provides services in parts of New England that lack 24/7 on-demand behavioral health clinicians in the emergency department and inpatient settings. 33% of pediatric patients are discharged to home after a consultation.
- The TeleICU team participates in approximately 4,000 video sessions per month, resulting in shorter hospital lengths of stay while often doubling the local ICU census.
- Two-thirds of deliveries involving TeleICN stayed local.
Patient Experience
Connected Care can improve the patient and family experience by keeping care closer to home, avoiding the time and cost of travel as well as lost wages from missing work, while also staying connected with local providers.
DH’s patients also are happy with telehealth care’s convenience and quality in the outpatient setting. Of patients surveyed regarding Connected Care’s Virtual Urgent Care service, 91% agreed that the care they received via telemedicine was as good as a regular in-person visit, and 97% reported being satisfied with the telemedicine care they received. One patient noted, “I live in a rural area. This service literally saved me spending my entire day dealing with this. Best thing ever.”
Lessons Learned
Connected Care is very conscious of the fact that clinicians at smaller rural hospitals are the true experts in providing care in their hospital and for their community. Dr. Curtis noted that fully appreciating the unique challenges of delivering care at a critical access hospital — which is often more difficult than at a larger referral center — goes a long way toward building relationships with hospitals and opening the door to information sharing and problem resolution. “We love figuring out how to solve clinical and operational problems together and often learn more from them than they do from us,” he said.
Looking Ahead
Connected Care leaders envision a sustainable telehealth infrastructure that addresses some of the core challenges of rural health care, including access to care, workforce shortages, quality, cost and transportation — while prioritizing care delivery close to home whenever possible. This vision extends beyond Northern New England, aiming to serve as a model for rural communities nationwide.
“It’s about the care, not the technology,” said Dr. Curtis. “Telehealth is a virtual extension of your team that can be embedded in the care experience.”