Comparison of Care in Hospital Outpatient Departments and Independent Physician Offices 2019-2024
Updated Findings for 2019-2024
Prepared for: American Hospital Association by KNG Health Consulting LLC
September 2025
Report Overview
- Study Background and Purpose
- Key Findings
- Overview of Study Approach
- Comparison of Patient Characteristics
- Conclusions
- Appendix: Data and Methodology
Study Background and Purpose
- Patients may receive non-emergent medical care in an independent physician’s office (IPO) or a hospital outpatient department (HOPD).
- Currently, Medicare pays different rates for the same service depending on the site of care.
- Some in Congress are considering policy recommendations to reduce differential payments for services delivered in the two settings.
- Whether a payment differential is appropriate depends on differences between IPOs and HOPDs.
- It has been documented that HOPDs face greater regulatory requirements,1 but less is known about the differences between the patients served in the two settings.
- This study aims to update our 2020 study by examining characteristics of Medicare patients seen in HOPDs and IPOs in 2019-2024.
Research Question
How do Medicare beneficiaries cared for in HOPDs and IPOs differ?
- Demographics and socioeconomic status
- Severity and medical complexity
- Prior healthcare utilization
Key Findings
- Compared to Medicare beneficiaries with cancer treated in IPOs, beneficiaries with cancer receiving care in HOPDs are more likely to be:
- Under 65 and disabled2
- Dually eligible
- From lower-income areas and rural counties
- Burdened with more severe chronic conditions
- Previously hospitalized
- Previously cared for in an emergency department
Overview of Study Approach
Study Overview
- Data Source: 2018Q4-2024Q2 Medicare Inpatient, Outpatient, and Carrier Standard Analytical Files and Denominator files.
- 2018Q4 is included only for a 90-day look-back period for utilization measures
- Study population: Had at least one HOPD or IPO visit between 1/1/2019 and 6/30/2024 & had continuous enrollment in Medicare FFS Part A & B in a given year and three months prior to the year
- Identifying HOPD and IPO Patients: A patient is considered an HOPD (IPO) patient in a given year if more than 50% of ambulatory care in that year is provided in HOPDs (IPOs).
| Study Question | Characteristics | Level of Analysis |
|---|---|---|
| How do Medicare patients cared for in HOPDs and IPOs differ? | Demographics | Patient Level |
| Socioeconomic Status | ||
| Clinical Characteristics | ||
| Prior Healthcare Utilization | Claim Level |
How Do Medicare Beneficiaries Cared for in HOPDs and IPOs Differ?
Relative to beneficiaries seen in IPOs, beneficiaries seen in HOPDs are . . .
54% More Likely to be under 65 and Disabled3
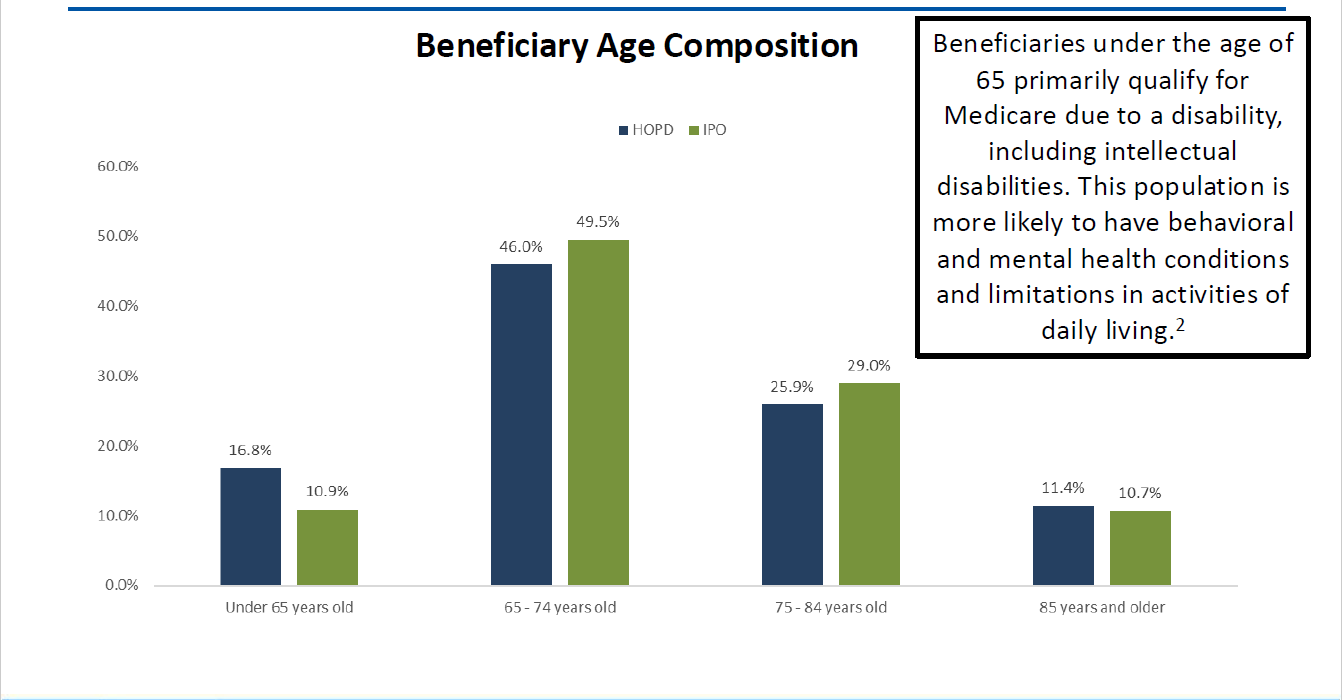
Source: KNG Health Consulting, LLC analysis of 2018Q4-2024Q2 Medicare claims data.
Beneficiaries under the age of 65 primarily qualify for Medicare due to a disability, including intellectual disabilities. This population is more likely to have behavioral and mental health conditions and limitations in activities of daily living.4
61% More Likely to be Dual Eligible
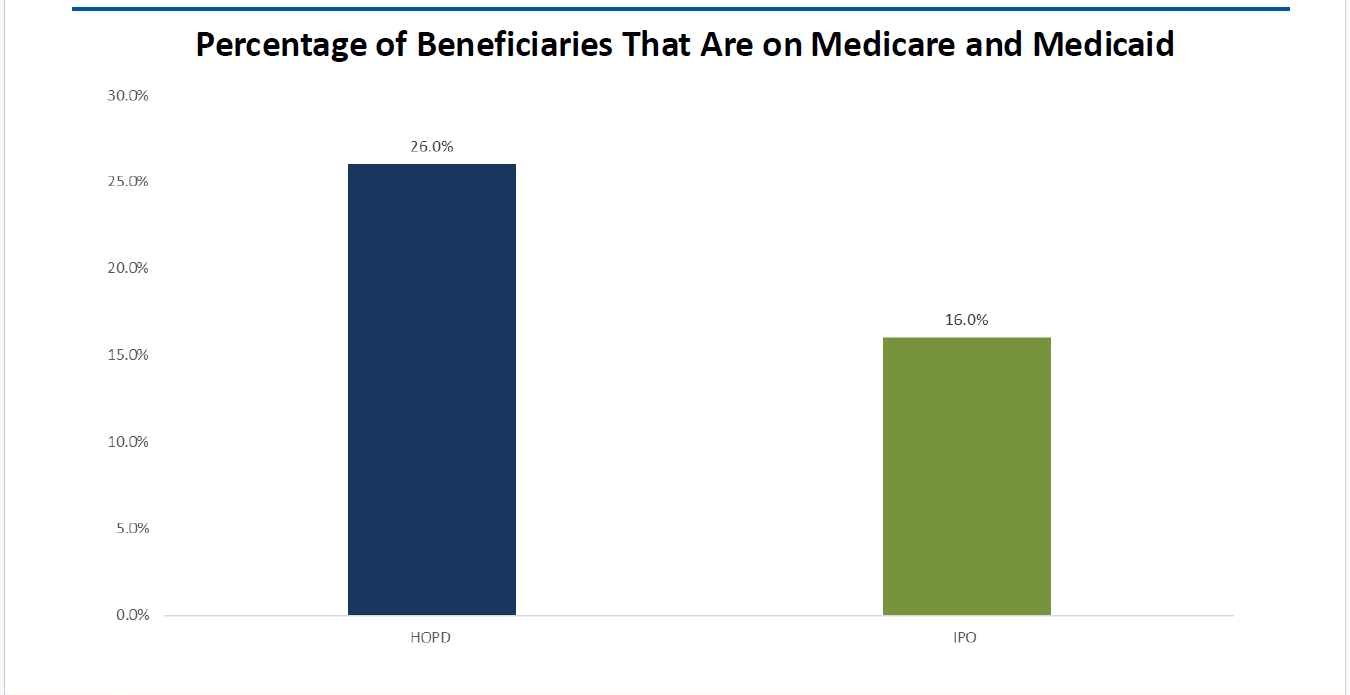
Source: KNG Health Consulting, LLC analysis of 2018Q4-2024Q2 Medicare claims data.
On Average, From Lower Income Areas
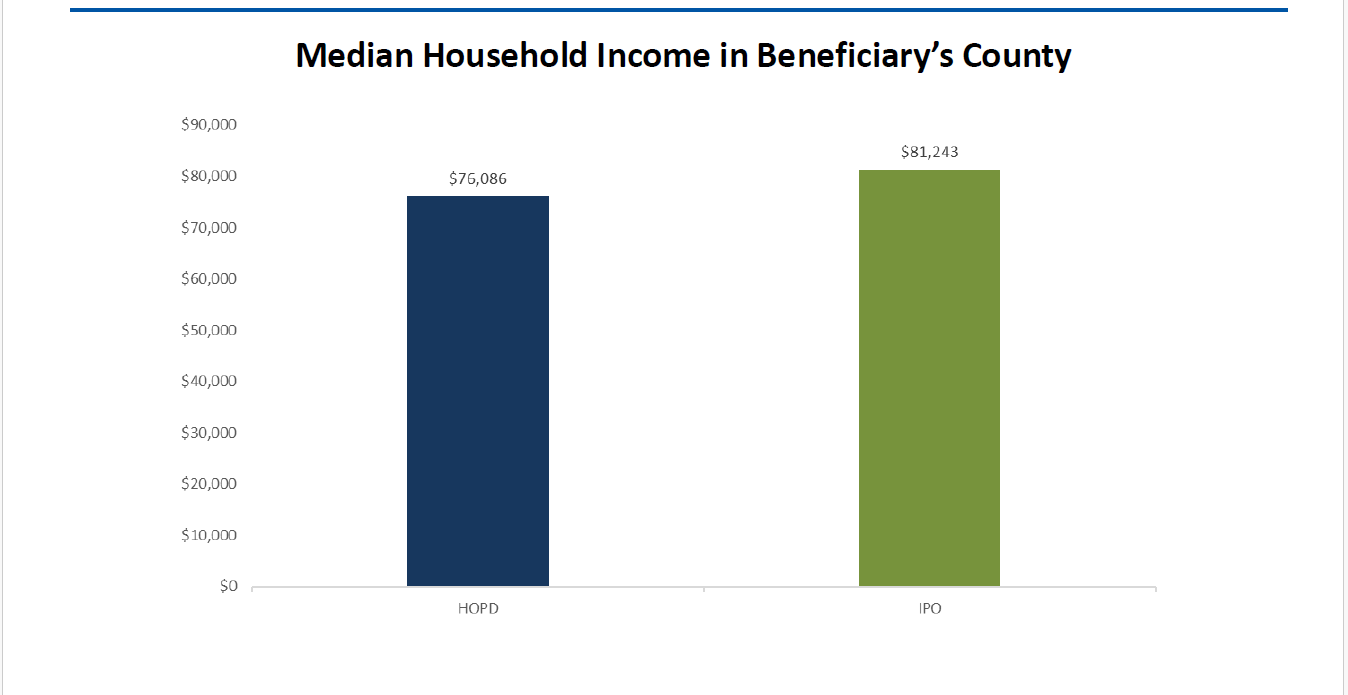
Source: KNG Health Consulting, LLC analysis of 2018Q4-2024Q2 Medicare claims data.
Median income is inflation adjusted and expressed in 2023 dollars.
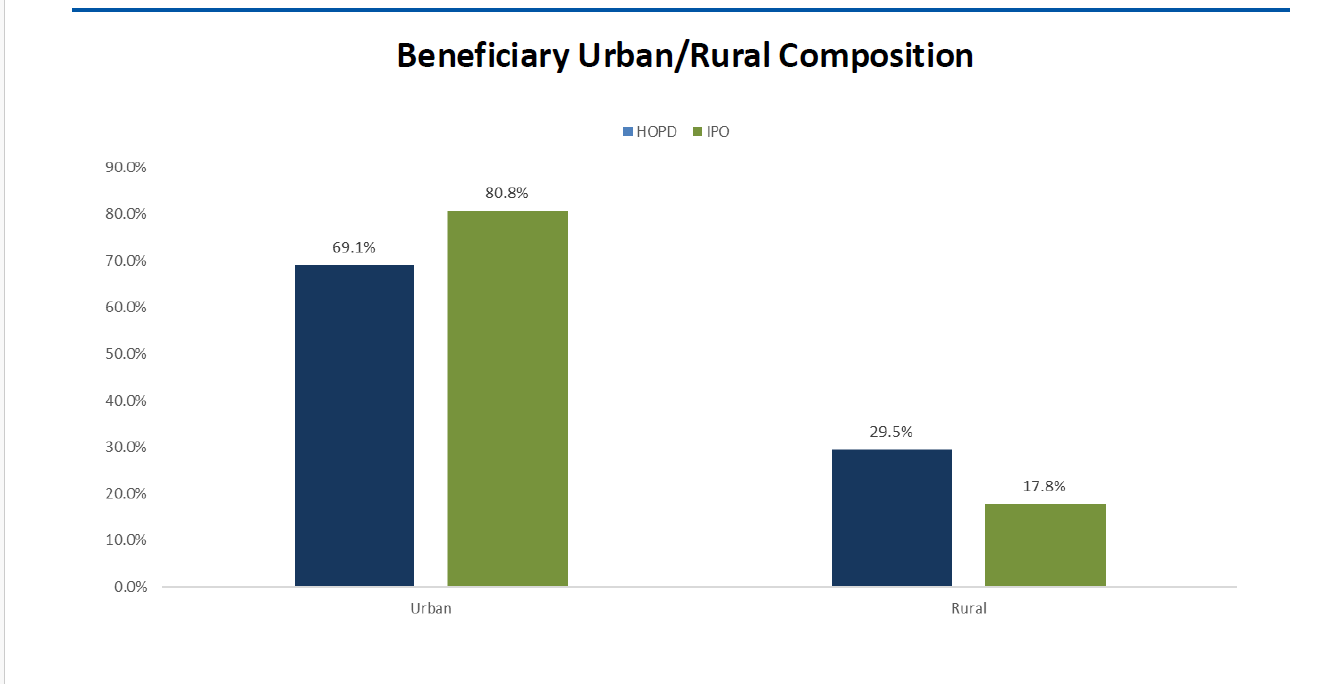
60% More Likely to Live in a Rural County
Source: KNG Health Consulting, LLC analysis of 2018Q4-2024Q2 Medicare claims data.
Note: Percentages may not add up to 100% due to “Unknown” county which is not depicted.
Severity and Complexity Measures
- We measured patient severity and complexity using three types of indicators: Charlson Comorbidity Index, number of complications/ comorbidities (CCs) and major CCs (MCCs), and prior utilization of care.
- The Charlson Comorbidity Index is a measure of patient severity computed by assigning higher weights to more severe conditions in terms of their effect on mortality.
- The Charlson Comorbidity Index includes 17 medical conditions that are found to be associated with 1-year mortality. A weight of 1 to 6 is assigned to each condition based on mortality risk, and weights are added across conditions to calculate total score.5,6
- The score is predictive of mortality, with 1-year and 10-year mortality rates greater than 50% for those with scores above 2.5,7
- Prior utilization of care captures inpatient hospital stays and emergency department visits in the 90 days preceding a HOPD or IPO visit.
Medicare Beneficiaries Seen in HOPDs Are Even Sicker
- The severity of chronic conditions as measured by the Charlson Comorbidity Score is y higher for beneficiaries seen in HOPDs.
- A greater percentage of HOPD patients have CCs and MCCs.
| Indicator | HOPD | IPO |
|---|---|---|
| Average Charlson Comorbidity Score | 2.80 | 2.08 |
| % with at least one CC | 57% | 48% |
| % with at least one MCC | 25% | 15% |
Medical conditions captured in Charlson Score: myocardial infarction, congestive heart failure, peripheral vascular disorders, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatic disease, peptic ulcer disease, mild liver disease, diabetes without chronic complication, diabetes with chronic complication, hemiplegia or paraplegia, renal disease, any malignancy (including lymphoma and leukemia, except malignant neoplasm of skin), moderate or severe liver disease, metastatic solid tumor, AIDS/HIV.
Source: KNG Health Consulting, LLC analysis of 2018Q4-2024Q2 Medicare claims data.
Note: CC = complications and comorbidities; MCC = major complications and comorbidities.
Medicare Beneficiaries Seen in HOPDs Have Higher Prior Emergency Department Use
| Emergency Department (ED) Use Prior to Visit | HOPD | IPO |
|---|---|---|
| Percent of HOPD/IPO Visits with a Prior ED Visit | 26% | 15% |
| Mean Number of ED Visits | 0.45 | 0.21 |
| Mean Number of ED Visits (Conditional on Having At Least 1 ED Visit) | 1.73 | 1.40 |
Source: KNG Health Consulting, LLC analysis of 2018Q4-2024Q2 Medicare claims data.
Medicare Beneficiaries Seen in HOPDs Have Higher Prior Inpatient Hospital Use
| Inpatient Hospital Use Prior to Visit | HOPD | IPO |
|---|---|---|
| Percent of HOPD/IPO Visits with a Prior Inpatient Hospital Stay | 15% | 7% |
| Mean Number of Inpatient Hospital Stays | 0.21 | 0.09 |
| Mean Number of Inpatient Hospital Stays (Conditional on Having at Least 1 Inpatient Hospital Stay) | 1.38 | 1.21 |
| Mean Total Inpatient Hospital Days (Conditional on Having at Least 1 Inpatient Hospital Stay) | 7.65 | 5.12 |
| Mean Total Inpatient Hospital Payments (Conditional on Having at Least 1 Inpatient Hospital Stay), in 2024 dollars | $26,988 | $19,106 |
Source: KNG Health Consulting, LLC analysis of 2018Q4-2024Q2 Medicare claims data.
Conclusions
- Our findings suggest key differences between Medicare beneficiaries treated in HOPDs and IPOs.
- Medicare beneficiaries primarily treated in HOPDs as compared to IPOs are more likely to
- be under 65 and disabled8
- be dual eligible.
- come from communities with lower income and reside in rural counties
- have more severe chronic conditions and higher prior utilization of hospitals and emergency departments
- Patients of higher complexity may require a greater level of care than patients of lower complexity.
- To the extent that these differences result in variations in the cost of care, site neutral payments may have adverse effects on patient access to care.
Appendix: Data and Methodology
Data and Study Population
- 2018Q4-2024Q2 Standard Analytical File of 5% sample of Medicare beneficiaries. Claims include:
- Inpatient
- Outpatient
- Professional services (Carrier file)
- The patient population consists of Medicare beneficiaries who fulfill the following criteria:
- Had at least one HOPD or IPO visit between Jan. 1, 2019 and Jun. 30, 2024.
- Had continuous enrollment in Medicare FFS Part A and Part B in a given calendar year and three months prior to the year.
Identification of HOPD and IPO Patients
- HOPD visits are identified using:
- Outpatient claims, excluding non-hospital claims, emergency department visit claims, and observation stay claims
- Carrier claims with place of service code of “22=Outpatient Hospital” or “19=Off-campus Outpatient Hospital”
- IPO visits are identified using:
- Carrier claims with place of service code of “11=Office”
- Identification of HOPD and IPO patient populations:
- A patient is considered an HOPD (IPO) patient in a given year if more than 50% of care in that year is provided in HOPDs (IPOs).
- Only HOPD claims for HOPD patients and IPO claims for IPO patients are included in the analysis.
Methodology: Descriptive Analysis
- Demographic, socioeconomic, and clinical characteristics were examined at the beneficiary level.
- Demographic characteristics: Obtained from the Medicare Denominator File.
- Socioeconomic characteristics of beneficiary’s county of residence: U.S. Census estimates of county-level characteristics based on 2023 American Community Survey are used. The 2023 Rural-Urban Continuum Codes were used to classify counties as urban vs. rural.
- Clinical characteristics: Charlson comorbidity index and number of CCs and MCCs are measured using diagnostic information from all inpatient, outpatient, and carrier claims that a patient had in a given year.
- Prior utilization was examined at the visit level.
- Prior utilization within 90 days prior to HOPD or IPO visit
- Emergency Department utilization: Emergency Department use is identified by revenue center codes 0450-0459, and 0981 in outpatient and inpatient claims files.
- Inpatient hospital utilization
Methodology: Statistical Analysis
- Differences between HOPDs and IPOs in terms of patient characteristics:
- T-tests were conducted to assess differences in average characteristics between the two settings using data from all years (2018Q4-2024Q2)
- All differences between HOPDs and IPOs presented in this report are statistically significant at the 0.1% level.
- American Hospital Association (2014). “Hospital Outpatient Department (HOPD) Costs Higher Than Physician Offices Due to Additional Capabilities, Regulations.”
- Medicare Beneficiaries under 65 are individuals with certain disabilities, end-stage renal disease, or amyotrophic lateral sclerosis (ALS). (https://www.cms.gov/Medicare/Eligibility-and-Enrollment/OrigMedicarePartABEligEnrol/index.html)
- Medicare Beneficiaries under 65 are individuals with certain disabilities, end-stage renal disease, or amyotrophic lateral sclerosis (ALS). (https://www.cms.gov/Medicare/Eligibility-and-Enrollment/OrigMedicarePartABEligEnrol/index.html)
- Lyons B, Andrews J, Claypool H. The Challenge Of Medicare And Medicaid Integration For Dual Eligible Individuals Under 65. Health Affairs Forefront (2025). Doi: 10.1377/forefront.20250220.305666
- Charlson, M. E., Pompei, P., Ales, K. L., & MacKenzie, C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases, 40(5), 373-383.
- Quan, H., Sundararajan, V., Halfon, P. et al. (2005). Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005 Nov;43(11):1130-9.
- Hall, W. H., Ramachandran, R., Narayan, S., Jani, A. B., & Vijayakumar, S. (2004). An electronic application for rapidly calculating Charlson comorbidity score. BMC Cancer,4(1), 94.
- Medicare Beneficiaries under 65 are individuals with certain disabilities, end-stage renal disease, or amyotrophic lateral sclerosis (ALS). (https://www.cms.gov/Medicare/Eligibility-and-Enrollment/OrigMedicarePartABEligEnrol/index.html)