The Growing Impact of Medicare Advantage on Rural Hospitals Across America
Executive Summary
Rural hospitals play a vital role in the health and economic stability of their communities, serving as lifelines for care and major local employers. However, these hospitals face mounting financial pressures
that jeopardize their ability to provide essential services.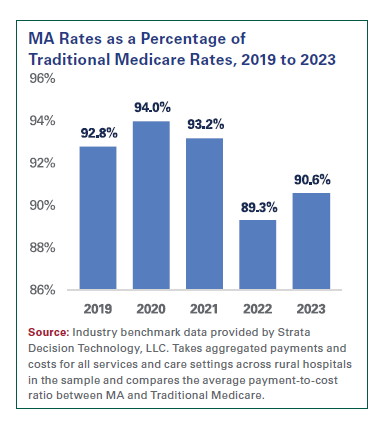
- The Medicare Advantage (MA) program has expanded rapidly and now accounts for more than half of total Medicare enrollment. While MA offers some benefits, certain plans reimburse hospitals below cost, delay or deny payments, and impose significant administrative hurdles, especially to rural hospitals, which have seen the fastest growth in MA recently. These risks exacerbate existing challenges like staffing shortages and unfavorable payer mixes. Over 100 rural hospitals have closed or converted to other provider types in the last decade, and according to Dobson DaVanzo & Associates, LLC, 429 rural hospitals are at high financial risk.1 Addressing the impact of MA on rural hospital finances is critical to safeguarding care access for millions of Americans in underserved areas.
This report explores how certain MA plans’ practices exacerbate rural hospitals’ vulnerability and threaten health care access for rural communities. Here are the report’s key findings:
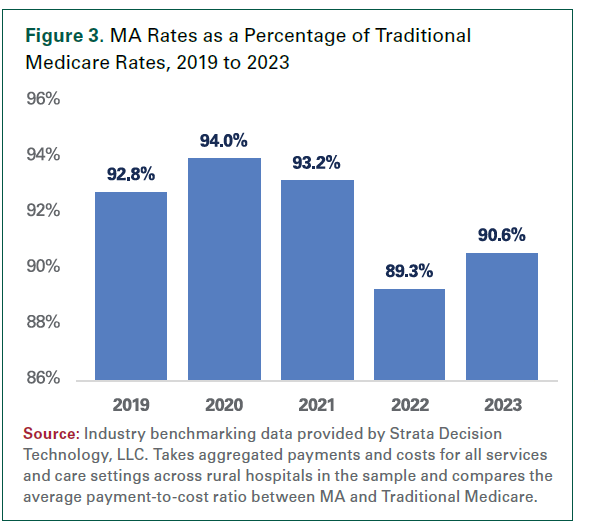
- Reimbursement well below the cost of care: Traditional Medicare often pays less than the cost of care, and increasingly rural hospitals report that MA plans pay even less — only 90.6% of Traditional Medicare rates on a cost basis, according to industry benchmark data provided by Strata Decision Technology, LLC (see chart).
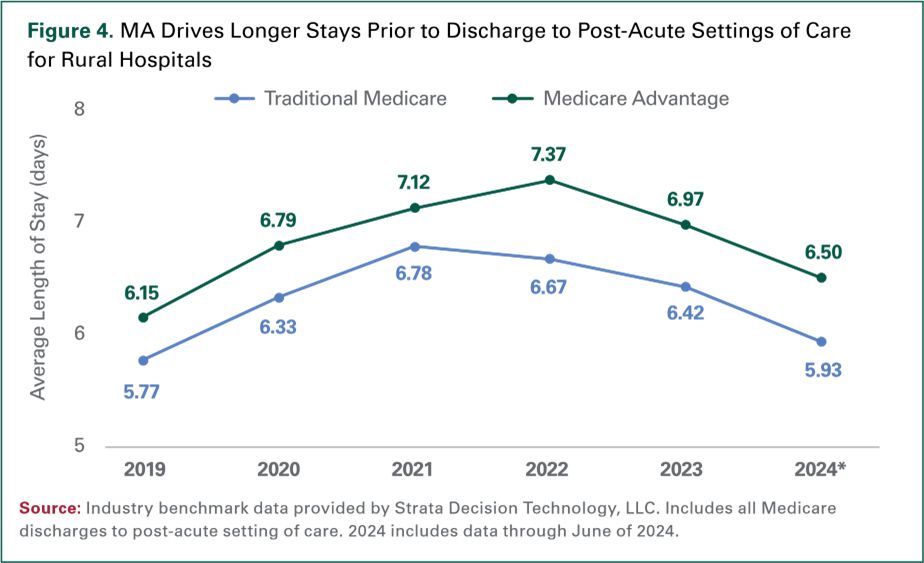
- Diminished access to quality care: Delays, denials, and excessive prior authorization from certain MA plans can hinder timely care: 81% of rural clinicians report quality reductions due to insurer requirements, and MA patients face 9.6% longer stays before post-acute care compared to similar Traditional Medicare patients.
- Administrative burdens and payment challenges: Delayed or denied MA payments worsen rural hospitals’ finances and increase administrative burdens. Nearly 4 in 5 rural clinicians report higher administrative tasks in five years, with 86% seeing negative impacts to patient outcomes.
Medicare enrollees will continue to choose MA plans and, as enrollment grows, it is ever more important that the program works both for the enrollee and the providers who care for them. Unsustainable reimbursement rates and administrative burdens strain these hospitals’ ability to deliver critical care in underserved areas. Meaningful oversight and reform are needed to ensure rural hospitals receive fair, timely reimbursement and can continue delivering high-quality care to their communities.
Introduction
Hospitals and health systems play a vital role in supporting the health and well-being of rural communities across the United States. They also serve as key economic drivers, creating jobs and stimulating local economic growth. Despite their critical importance, rural hospitals face a host of financial challenges that threaten access to care for the 46 million Americans living in rural areas.2 Many of these difficulties have been well documented, including staffing shortages, low patient volumes and heavy reliance on payers that reimburse below the cost of care.3 Less recognized, however, is the impact of the rapid expansion of Medicare Advantage (MA) plans and the impact of certain MA practices on rural hospitals. Based on both quantitative and qualitative analyses, including interviews with rural hospital leaders, this report finds that the practices used by some MA plans pose several distinct risks to rural communities:
- Reimbursement well below the cost of care: Traditional Medicare is broadly recognized as paying below the cost of care.4 Increasingly, rural hospitals report that MA plans pay even less. Industry benchmark data provided by Strata Decision Technology, LLC shows that MA plans reimburse rural hospitals at just 90.6% of Traditional Medicare rates on a cost basis.
- Diminished access to quality care: Excessive insurer delays and denials of care as well as cumbersome prior authorization requirements from certain MA plans interfere with clinicians’ ability to provide timely and effective care. For example, 81% of rural clinicians report reduced quality of care due to insurer requirements, and MA patients experience longer lengths of stay — 9.6% longer on average before discharge to post-acute care — compared to clinically-similar Traditional Medicare patients.
- Administrative burdens and payment challenges: Delayed or denied payments by certain MA plans compound financial difficulties for rural hospitals, including by adding substantial administrative costs. Nearly 4 in 5 rural clinicians report significant increases in administrative tasks over the past five years, with 86% reporting this leading to negative impacts on patient outcomes.5
Each of these challenges disproportionately strain rural hospitals with limited resources and persistent staffing shortages. Rural hospitals already contend with a challenging payer mix as they disproportionately serve older, sicker patients who are more likely to be covered by Medicare or Medicaid — programs that typically reimburse well below the cost of care. Facing MA’s below-cost reimbursements, many rural hospitals may lack the leverage to negotiate better rates with large, national insurers, leaving them forced to accept unsustainable contracts.
Ultimately, growth in MA enrollment is compounding the financial pressure on rural hospitals, which are already struggling to stay afloat.6 Over 100 rural hospitals have closed or converted to other provider types in the last decade, and according to Dobson DaVanzo & Associates, LLC, 429 rural hospitals are at high financial risk.7 Meanwhile, MA enrollment in rural areas has surged, quadrupling since 2010.8 At its current growth rate, MA enrollment is projected to surpass half of all rural Medicare enrollment by this year.9
Given the growing presence of MA plans in rural communities, meaningful reforms are needed to ensure fair and timely reimbursement and reduce the excessive administrative burden on rural providers. Without these changes, this added financial pressure may force more rural hospitals to cut services or close altogether, further limiting health care access in already underserved communities.
The Rise of MA and Associated Challenges for Rural Hospitals
Over the past decade, total MA enrollment in the U.S. has surged by 120%, increasing from 15 million beneficiaries in 2014 to 33 million in 2024 — or 54% of total Medicare enrollment. The Congressional Budget Office (CBO) projects that by 2034, MA will cover 64% of all Medicare beneficiaries.10
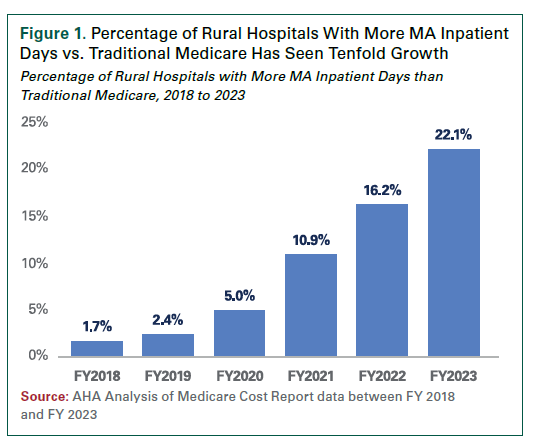
In rural areas, MA penetration has reached or exceeded 50% of the Medicare market in an increasing number of counties.11,12 Nationwide, the proportion of hospitals with more MA inpatient days than Traditional Medicare inpatient days nearly tripled over a five-year period ending in 2023. This shift is more striking in rural hospitals, where the share grew by more than tenfold (see Figure 1).
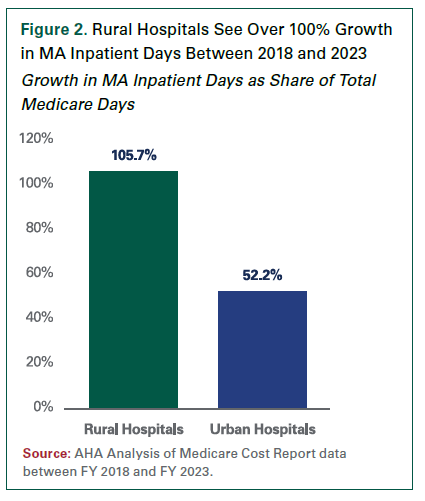
For rural hospitals, the share of MA inpatient days as a proportion of all Medicare inpatient days more than doubled over that same period (105.7%), outpacing the 56% growth seen across all hospitals (see Figure 2).13
The growth of MA enrollment in rural areas can be attributed to several factors. Broadly, many beneficiaries may choose to enroll in an MA plan to receive supplemental benefits, such as cost-sharing protections (e.g., out-of-pocket maximum limits) and/ or medical benefits (e.g., vision, hearing and dental), that are not available under Traditional Medicare. In other cases, employers may offer MA plans as a retirement benefit with the same insurer as used for individuals’ employer-sponsored coverage, helping promote continuity of care. Furthermore, in 2020, the Centers for Medicare & Medicaid Services (CMS) issued regulatory changes that loosened network adequacy standards for MA plans in rural areas, with further flexibilities provided to rural MA plans that included certain types of telehealth providers in their networks. These changes helped increase the number of MA plans with compliant networks in rural areas and led to an expanded number of MA plan options for rural beneficiaries.
However, this rapid expansion has left stakeholders and policymakers grappling with its implications for the health care system. Several concerns have already emerged regarding the practices of certain MA plans. Investigations have revealed that these plans frequently use claim denials, prior authorization requirements and other administrative tactics that delay or deny care to patients, which in turn delays and denies payments to hospitals.14 Inadequate reimbursement for services that these plans do cover further compounds hospital losses.
MA’s Eroding Payments to Rural Hospitals
Many MA plans reimburse hospitals, including those in rural areas, at lower rates than Traditional Medicare, which already pays below the cost of care. An AHA analysis using industry benchmark data provided by Strata Decision Technology, LLC found that in 2023 MA plans reimbursed rural hospitals at just 90.6% of Traditional Medicare rates on a cost basis (see Figure 3).
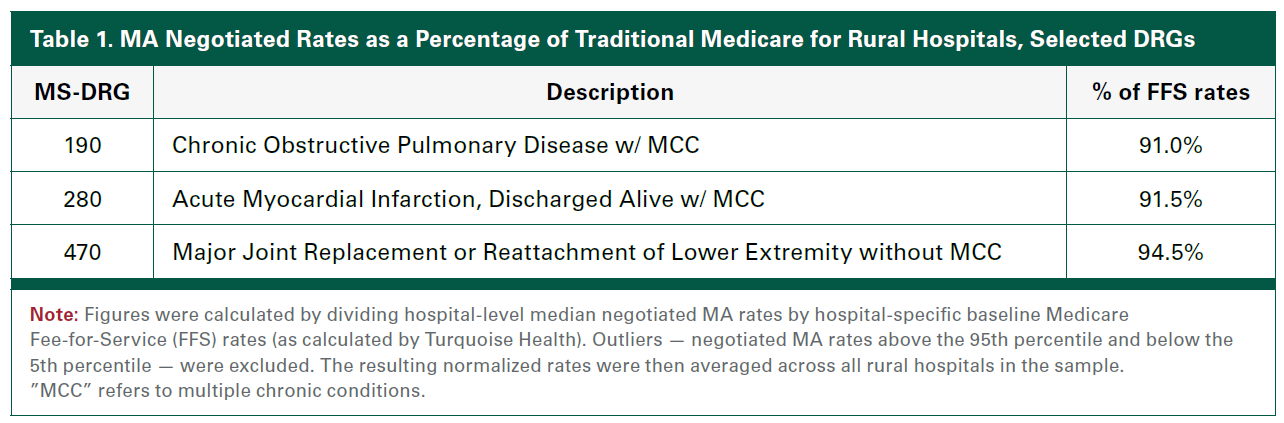
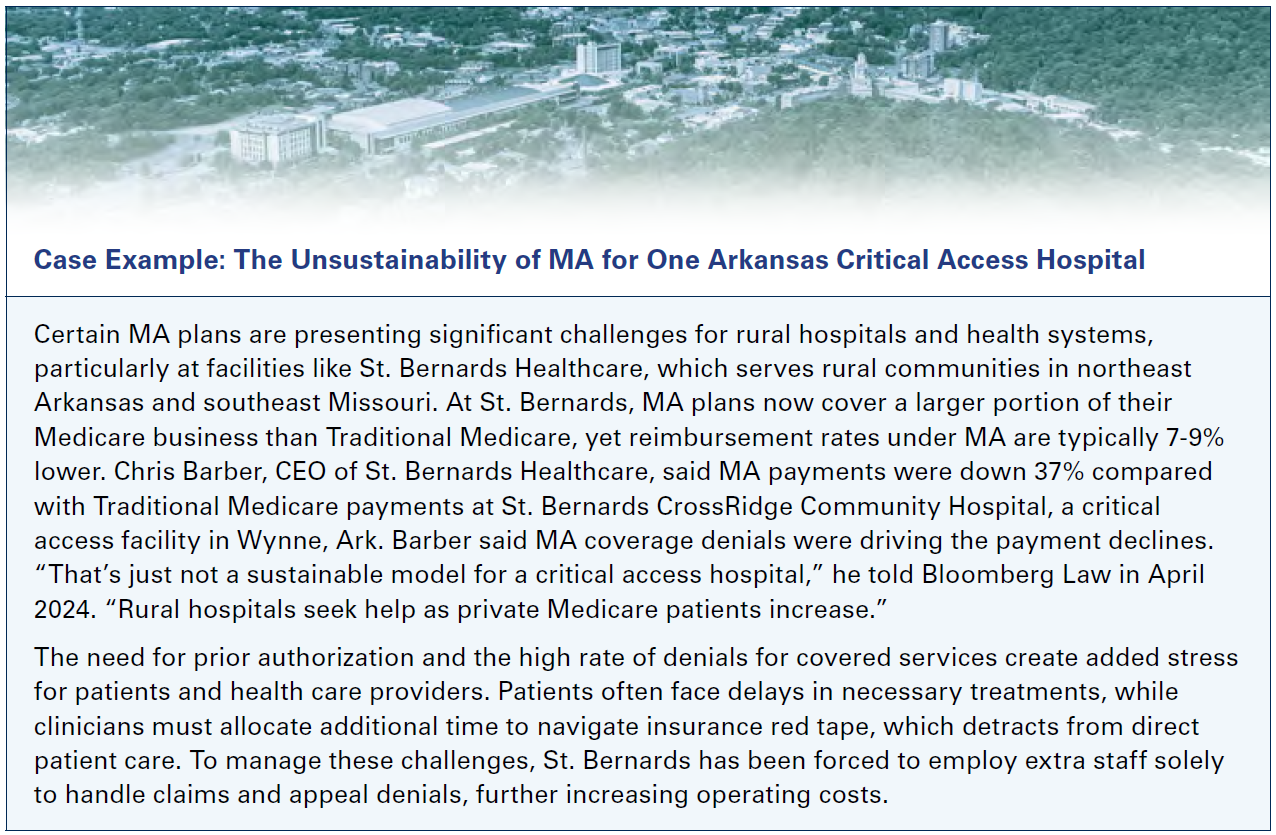
 These lower payment-to-cost ratios can be attributed to both higher non-clinical costs associated with treating MA patients (due in part, for example, to longer lengths of stay for MA enrollees as a result of post-acute care prior authorization delays) and lower reimbursement rates. An AHA analysis of hospital prices using price transparency data from Turquoise Health15 found that average MA rates for common Medicare Severity Diagnosis Related Groups (MS-DRGs) fell between 91% and 94.5% of hospital-specific Traditional Medicare rates (see Table 1). And the trend is worse for certain types of rural hospitals. For example, in 2023, Medicare dependent and low-volume hospitals received average MA rates amounting to just 85% of what they would have received under Traditional Medicare, according to industry benchmark data provided by Strata Decision Technology, LLC. Even critical access hospitals (CAHs), which are reimbursed by Traditional Medicare based on the cost of care, received only 95% of Traditional Medicare rates from MA plans on a cost basis, according to industry benchmark data provided by Strata Decision Technology, LLC. This can result in effectively undermining the intent of the CAH program. Overall, the AHA estimates that this lack of payment parity cost rural hospitals over $1 billion in 2023. Those losses are only expected to climb.
These lower payment-to-cost ratios can be attributed to both higher non-clinical costs associated with treating MA patients (due in part, for example, to longer lengths of stay for MA enrollees as a result of post-acute care prior authorization delays) and lower reimbursement rates. An AHA analysis of hospital prices using price transparency data from Turquoise Health15 found that average MA rates for common Medicare Severity Diagnosis Related Groups (MS-DRGs) fell between 91% and 94.5% of hospital-specific Traditional Medicare rates (see Table 1). And the trend is worse for certain types of rural hospitals. For example, in 2023, Medicare dependent and low-volume hospitals received average MA rates amounting to just 85% of what they would have received under Traditional Medicare, according to industry benchmark data provided by Strata Decision Technology, LLC. Even critical access hospitals (CAHs), which are reimbursed by Traditional Medicare based on the cost of care, received only 95% of Traditional Medicare rates from MA plans on a cost basis, according to industry benchmark data provided by Strata Decision Technology, LLC. This can result in effectively undermining the intent of the CAH program. Overall, the AHA estimates that this lack of payment parity cost rural hospitals over $1 billion in 2023. Those losses are only expected to climb.
The implications of this payment disparity are far reaching. Rural hospitals rely more heavily on total Medicare revenues to maintain their operations. While Medicare made up 37% of total hospital revenues nationwide in 2023, it accounted for 43% of revenues for rural hospitals.16 Consequently, rural hospitals are more reliant on revenues from MA than ever before. In fact, over the last five years, MA revenues as a share of total Medicare revenues have grown from 11.4% to 17.6%.17
Administrative Burden Impacts on Costs and Patient Access to Care in Rural Communities
Adding to these financial strains, rural hospitals are grappling with increasing administrative burdens driven by the operational practices of certain MA plans. For example, a Kaiser Family Foundation report found that prior authorization requests in MA surged to nearly 50 million in 2023, a 43.9% increase from 2020.18 And despite these authorizations, hospitals face increasing care denials and withheld payments for essential care.19 For rural hospitals that often operate with limited staffing, technology  and other resources, these practices present substantial challenges to their workflow and budgets, while patients face delays and uncertainty in receiving timely care.
and other resources, these practices present substantial challenges to their workflow and budgets, while patients face delays and uncertainty in receiving timely care.
Care delays often mean increased costs for hospitals and health systems, particularly when plans prevent hospitals and health systems from discharging patients in a timely manner to the next site of care. A recent report by the Senate Permanent Subcommittee on Investigations found that certain MA plans disproportionately targeted post-acute care facilities with claim denials and prior authorization requirements.20 In fact, an AHA analysis of industry benchmark data provided by Strata Decision Technology, LLC revealed that in 2024, rural hospital patients covered by MA plans experienced an average length of stay 9.6% longer prior to discharge to a post-acute care setting compared to those covered by Traditional Medicare (see Figure 4). This represents a 46% growth in the difference in average length of stay for MA patients relative to Traditional Medicare between 2019 and 2024.
Care delays and denials also can have a cascading effect on health outcomes for patients. A recent AHA survey conducted by Morning Consult found that 81% of clinicians practicing in rural communities reported reductions in quality of care to patients as a result of insurer administrative requirements. Sadly, MA enrollees experience a disproportionate number of these delays. A Commonwealth Fund survey found that 22% of MA enrollees experienced care delays due to prior authorization, nearly double the rate for Traditional Medicare (13%).21 Similarly, a 2022 Health and Human Services Office of Inspector General report revealed that MA plans inappropriately denied up to 85,000 prior authorization requests in 2019 and rejected nearly 20% of reimbursement claims that met Medicare coverage rules.22 These inappropriate denials also impose a staggering financial toll on hospitals, which collectively spend an estimated $20 billion annually contesting health plan denials.23
In addition, these administrative burdens also weigh heavily on hospitals’ staff — the nurses, physicians, therapists, financial counselors and others — exacerbating burnout and diminishing the quality of care. This burden ultimately makes it more challenging for rural hospitals to staff these positions. The same AHA survey conducted by Morning Consult found that nearly 4 in 5 clinicians in rural communities report increases in insurer-required administrative tasks over the past five years, with over half describing this burden as high or extremely high. Alarmingly, 86% noted negative impacts on patient outcomes. Such findings underscore the human cost of administrative burden, where increasing operational challenges directly undermine the mission of rural hospitals to deliver timely and effective care to their communities.
Conclusion
Medicare enrollees will continue to choose MA plans and, as enrollment grows, it is ever more important that the program works both for the enrollee and the providers who care for them. The growing presence of MA plans in rural communities presents significant challenges for rural hospitals. As MA plans reimburse rural hospitals at unsustainable rates and impose administrative hurdles, they continue to strain hospitals’ ability to provide critical services in underserved areas. Meaningful oversight and reform are needed to ensure rural hospitals receive fair, timely reimbursement and can continue delivering highquality care to their communities.
In response, several bipartisan bills have been introduced to better regulate MA prior authorization processes and alleviate the arduous paperwork burden placed on hospitals serving MA patients. Additionally, a CMS rule clarified “clinical criteria guidelines to ensure people with MA receive access to the same medically necessary care they would receive in Traditional Medicare.” However, hospitals have noted little improvement since the rule’s finalization in January.24
Here are several AHA recommendations:
- Streamline prior authorization processes to protect timely access to medical care and drugs covered under the medical benefit. To accomplish this, the AHA supports the Improving Seniors’ Timely Access to Care Act, which would streamline prior authorization requirements in MA. The bill would make significant progress toward reducing complexity and promoting uniformity in prior authorization processes and requirements that frustrate both patients and providers. Additionally, the bill would significantly increase the specificity of prior authorization data reported by plans, which will give the Department of Health and Human Services greater insight into problematic plan processes and enable more targeted enforcement of policies designed to protect patient access to necessary care. The legislation also would apply provisions that streamline prior authorization to clinic-administered drugs covered under the medical benefit, such as injections typically used to treat cancer and other complex diseases.
- Cost-based reimbursement for CAHs from MA plans. Congress created a special statutory payment designation for CAHs in recognition of the unique role they play in preserving access to health care services in rural areas. As the MA program is growing rapidly in rural communities, this important financial protection is being eroded. Indeed, a greater portion of a CAH’s revenue is subject to negotiation with MA plans that often result in below-cost payment terms and involve onerous plan requirements that contribute to administrative burden, unnecessary delays and denials in approving and paying for patient care, as well as additional strains on the health care workforce. The AHA supports legislation to ensure CAHs receive cost-based reimbursement for MA patients.
- Ensure prompt payment from insurers for medically necessary, covered health care services delivered to patients. The AHA supports policies that would require timely payment to providers to ensure they have the resources they need to pay staff and acquire the supplies to care for patients.
- Require MA plan clinician reviewers who review coverage denials (adverse determinations) to provide their name and credentials and attest they meet existing CMS rules and have relevant training and expertise in the requested service. As health plans play an important role in patient care through their coverage policies, it is important that patients’ clinicians and regulators know who is making determinations that impact whether a patient can access the medically necessary care they need in a timely manner.
- Improve data collection, reporting and transparency in the MA program with a focus on metrics that are meaningful indicators of patient access, such as appeals, grievances and denials. These data will provide patients, state and federal regulators, and other stakeholders with the information necessary to hold health plans accountable for meeting their obligations to beneficiaries. These data could be used, for example, to target for audits those plans with inappropriate or questionable practices and identify and apply penalties to health plans that are noncompliant with federal rules.
- Expand network adequacy requirements for certain post-acute sites of care. To help mitigate the cost of caring for patients ready for discharge to post-acute care but who face health plan authorization delays, MA plans should be required to explicitly cover services in all post-acute sites of care. Specifically, inpatient rehabilitation facilities, long-term care hospitals and home health agencies25 should be added to MA network adequacy requirements and standards should be adopted to ensure there are a sufficient number and type of each PAC facility in MA networks.
End Notes:
____________________________________________________________
1 https://strengthenhealthcare.org/new-report-finds-integration-with-a-hospital-system-can-protect-rural-hospitals-patient-access-to-care/
3 https://www.aha.org/2022-09-07-rural-hospital-closures-threaten-access
4 https://www.medpac.gov/wp-content/uploads/2024/03/Mar24_MedPAC_Report_To_Congress_SEC-3.pdf
5 This poll was conducted by Morning Consult on behalf of the American Hospital Association (AHA) between October 30 – November 15, 2024, among a sample of 1,001 clinicians.
12 https://www.medpac.gov/wp-content/uploads/2024/03/Mar24_MedPAC_Report_To_Congress_SEC.pdf
13 AHA analysis of Medicare Cost Report data between FY 2018 and FY 2023.
15 The views and opinions expressed reflect only the AHA’s sentiment and do not necessarily reflect the official position of Turquoise Health.
16 AHA analysis of AHA Annual Survey data from 2023.
17 AHA analysis of AHA Annual Survey data between 2019 and 2023.
19 https://www.nbcnews.com/health/rejecting-claims-medicare-advantage-rural-hospitals-rcna121012
25 Skilled nursing facilities are already included in MA plan network adequacy requirements.