Burnout: The New Pandemic

Health care has always been a demanding profession, and the effects of the last few years have meant that health care workers have been asked to do more with less. Expectations have been higher than ever, while money, support staff and even basic rest and recuperation have not kept pace. That means that the field is now facing what could be a new pandemic: burnout.
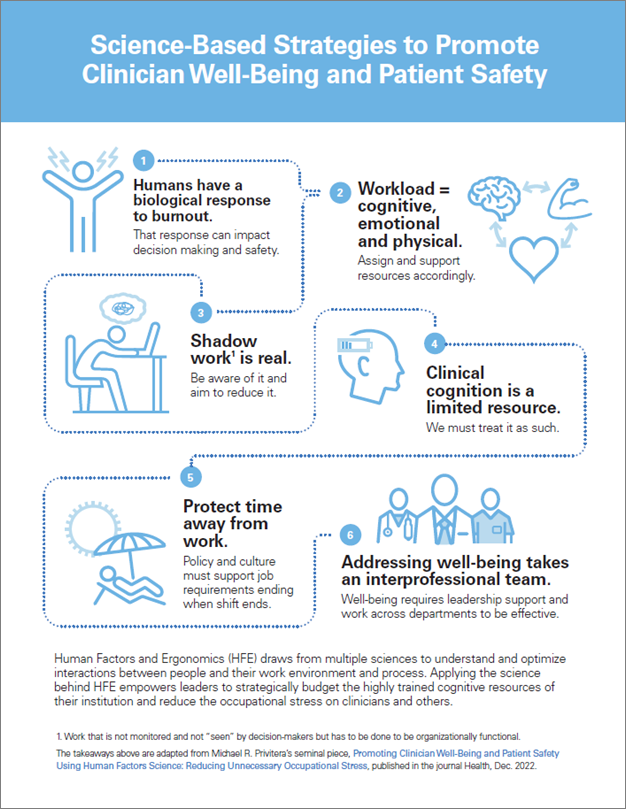
Burnout is not just feeling tired or stressed; it is a condition that affects the brain in very real, noticeable ways. It affects decision-making skills, memory, the ability to focus and even fine motor control – abilities that are vital at every level of the health care field. Combined with the stressors often found in health care, such as working night shifts, working for extended hours, intense working conditions, and sleep and food deprivation, burnout puts the mental and physical health of our workforce at risk. This graphic uses science to give a roadmap to reduce burnout and risk of medical error in organizations.
It is imperative to recognize that health care is a unique field in that it requires emotional, physical and cognitive labor, often all at the same time. If a nurse is physically exhausted, they cannot provide emotional support to their patients. If a doctor is emotionally depleted due to job (or any) stressors, they will not be operating at the top of their cognitive skill set.
Hospitals and health systems also must be aware of the “shadow work” that goes into health care – those duties that aren’t part of anyone’s job description, but can fill their day. While they are not reflected in metrics or on operational dashboards, they take time away from patient care, such as searching the EMR to accommodate for interface changes, documentation burdens that don’t add to care delivery or prior authorization requirements. Changes in staffing can further add cross coverage challenges.
Fortunately, burnout is both avoidable and reversible when hospitals and health systems are willing to take the steps to grow a culture in which every worker has access to ways to decrease stress. Primary coping is taking away the factors causing the stress. Secondary coping is finding ways to deal with the remaining factors that cause stress. Both are needed. Interventions that focus upon helping the individual with resilience are helpful but important to recognize that health care workers start off being more resilient than the average worker. Hence organizational or systemic interventions to improve the work environment are also needed.
Organizational health also leads to worker health. A structural focus on employees’ well-bring, clear processes and workflows, and a commitment to organizational justice are all factors that, when incorporated into a hospital’s organizational alignment, create a work environment in which employees (and therefore patients) can thrive, because they know they are valued and their work is respected.
Over the past few years, we have asked so much of our health care workforce. Now is the time for hospitals and health care systems to identify and enact the structural changes that will protect them, our patients, and the workforce in general.
Elisa Arespacochaga, AHA and Michael R Privitera, M.D. Professor Emeritus of Psychiatry, University of Rochester Medical Center