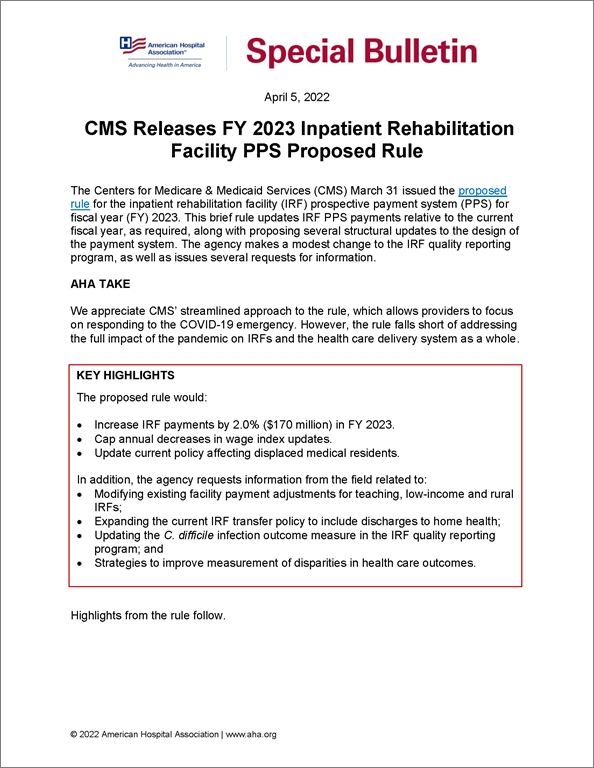
CMS Releases FY 2023 Inpatient Rehabilitation Facility PPS Proposed Rule
Special Bulletin
April 5, 2022
The Centers for Medicare & Medicaid Services (CMS) March 31 issued the proposed rule for the inpatient rehabilitation facility (IRF) prospective payment system (PPS) for fiscal year (FY) 2023. This brief rule updates IRF PPS payments relative to the current fiscal year, as required, along with proposing several structural updates to the design of the payment system. The agency makes a modest change to the IRF quality reporting program, as well as issues several requests for information.
AHA TAKE
We appreciate CMS’ streamlined approach to the rule, which allows providers to focus on responding to the COVID-19 emergency. However, the rule falls short of addressing the full impact of the pandemic on IRFs and the health care delivery system as a whole.
Key Highlights
The proposed rule would:
- Increase IRF payments by 2.0% ($170 million) in FY 2023.
- Cap annual decreases in wage index updates.
- Update current policy affecting displaced medical residents.
In addition, the agency requests information from the field related to:
- Modifying existing facility payment adjustments for teaching, low-income and rural IRFs;
- Expanding the current IRF transfer policy to include discharges to home health;
- Updating the C. difficile infection outcome measure in the IRF quality reporting program; and
- Strategies to improve measurement of disparities in health care outcomes.
Highlights from the rule follow.
IRF PPS PAYMENT CHANGES
Proposed FY 2023 Payment Update
The rule would increase net payments to IRFs by 2.0% ($170 million) in FY 2023 relative to FY 2022. This includes a 3.2% market-basket update offset by a statutorily-mandated cut of 0.4-percentage-point for productivity, and a 0.8-percentage-point cut for high-cost outlier payments. The latter would reduce the number of cases that qualify for an outlier payment with the goal of limiting total FY 2023 outlier payments at 3.0% of all IRF PPS payments that year, per current policy.
Proposed Permanent Cap on Wage Index Decreases
CMS proposes to adopt a permanent policy that would cap wage index decreases from year-to-year at 5%. CMS anticipates that this cap would rarely be used, but, when needed, would improve the stability of this payment system.
PROPOSED CHANGES RELATED TO THE FACILITY-LEVEL ADJUSTMENT FOR “TEACHING IRFS”
Proposed Changes Regarding Displaced Medical Residents
CMS proposes to update and clarify its current policy addressing medical residents (and interns) who are displaced when a teaching IRF closes. The rule would alter the status of a relocating resident based on the date that the originating IRF publicly announces its closure (for example, via a press release), rather than the actual closure date, which would mitigate delayed transfers of a displaced resident to a new IRF. In addition, the rule would allow the receiving IRF to increase its FTE resident cap by submitting a letter to its Medicare Administrative Contractor (MAC) within 60 days after beginning to train the displaced residents.
Proposed Codification of IRF Teaching Status Adjustment
To improve clarity, CMS is proposing to codify and consolidate existing policies related to reimbursement for IRFs providing graduate medical education.
PAYMENT-RELATED REQUESTS FOR INFORMATION (RFI)
IRF PPS Facility Level Adjustments
Currently, the IRF PPS adjusts payments based on an IRF’s percentage of low-income patients, teaching status, and rural status, to account for differences in costs attributable to these characteristics. Updates to these annual adjustments factors are made in a budget-neutral manner. To mitigate the impact of relatively large fluctuations in these factors from year-to-year, the adjustment levels have been frozen since FY 2014, with general support from the field. While CMS is not proposing a change for FY 2023, Table 9 in the rule shows what the annual facility adjustments would have been for FY 2015 through FY 2023, and demonstrates substantial volatility. This rule seeks comments from stakeholders to help better understand the cause of these fluctuations and consider how to best account for them in the future.
IRF Transfer Policy
CMS is also seeking feedback from the field on whether to incorporate a “discharge to home health” element in the IRF transfer policy in the future, in alignment with inpatient and inpatient psychiatric facility PPS policies. This policy, which is intended to disincentivize early discharges from IRFs, currently applies to stays with a less than average length-of-stay for cases with comparable principal and secondary diagnoses, which are transferred directly to another IRF, general acute-care hospital, or nursing home/SNF. This possible, future recommendation reflects a December 2021 report by the Department of Health and Human Services Office of the Inspector General report1, based on an audit of calendar year 2017 and 2018 Medicare claims, which found that this form of transfer policy expansion would generate savings of approximately $1 billion over two years.
IRF QUALITY REPORTING PROGRAM (QRP)
CMS proposes to require IRFs to report quality data, including the standardized patient assessment data in the IRF Patient Assessment Instrument (PAI), on all patients regardless of payer. If finalized, IRFs would be required to collect the IRF PAI for all patients beginning Oct. 1, 2023. The agency estimates that the increased burden will result in an additional average cost of $28,505.41 per IRF annually, at a total cost of over $31 million for the field per year.
CMS does not propose any other changes to the QRP, including any new quality measures.
QUALITY REPORTING-RELATED RFIS
CMS seeks stakeholder feedback on a number of topics, which the agency reports will influence the direction of the QRP in the future.
C. difficile Infection Outcome Measure
CMS requests input on the potential inclusion of an updated healthcare-associated infection measure in the IRF QRP. The measure, National Healthcare Safety Network (NHSN) Healthcare-associated Clostridioides difficile Infection (HA-CDI) Outcome Measure, improves upon the CDI measure currently used in the IRF QRP by using data from electronic health records. CMS purports that this method both increases the accuracy of the measure and reduces reporting burden, as it would negate manual entry of information into the NHSN reporting platform. In the RFI, CMS would like to assess the feasibility of this “digital” measure in IRFs.
Measuring Equity and Quality Disparities
Separately, CMS seeks feedback on its strategies to improve measurement of disparities in health care outcomes. In this RFI, the agency requests input on its framework to collect, stratify and report quality performance data across CMS programs as well as specific methods the agency could deploy within the IRF QRP specifically. The latter might include quality measures assessing a facility’s commitment to addressing health equity by taking on certain practices.
FURTHER QUESTIONS
CMS will accept comments on the IRF proposed rule through May 31. AHA’s IRF members will receive an invitation for a call to discuss the rule and inform AHA’s comments. Please contact Rochelle Archuleta, AHA director of policy, at rarchuleta@aha.org with any questions.
__________
1 Office of the Inspector General. December 7, 2021 Early Discharges From Inpatient Rehabilitation Facilities to Home Health Services [Report No. A-01-20-00501] https://oig.hhs.gov