How OR 'Black Boxes' Are Helping to Improve Safety
When Teodor Grantcharov, M.D., Ph.D., joined Stanford Medicine last April as professor of surgery, he brought with him a valuable skill set in safety improvement research.
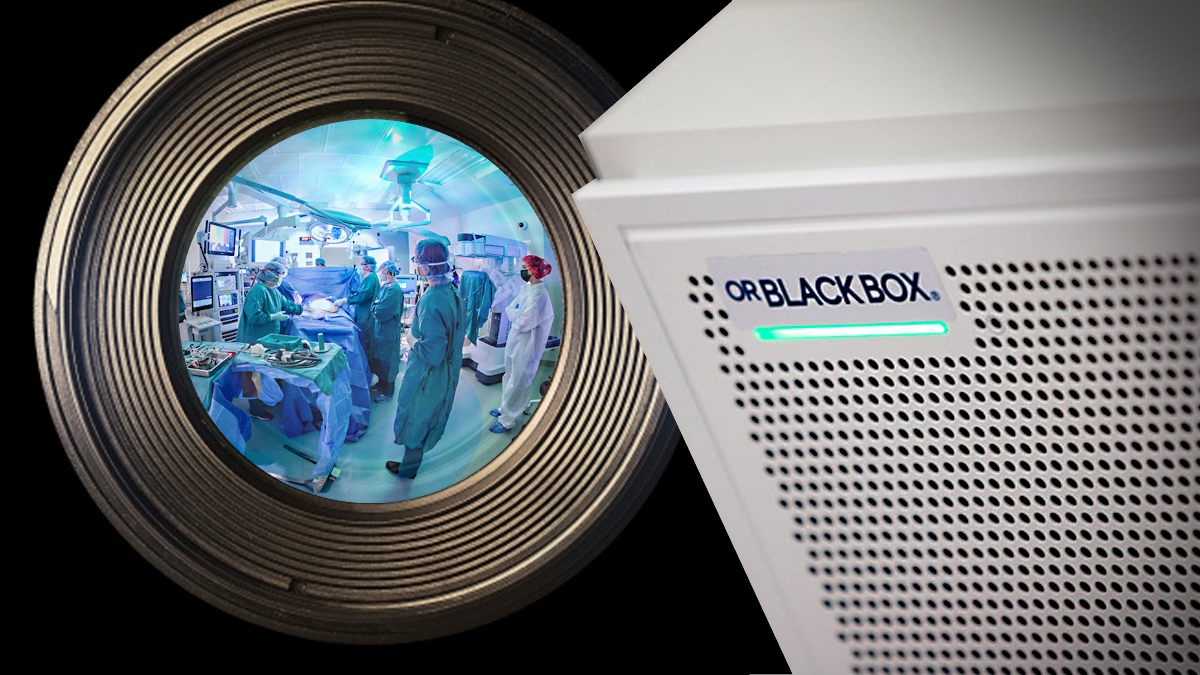
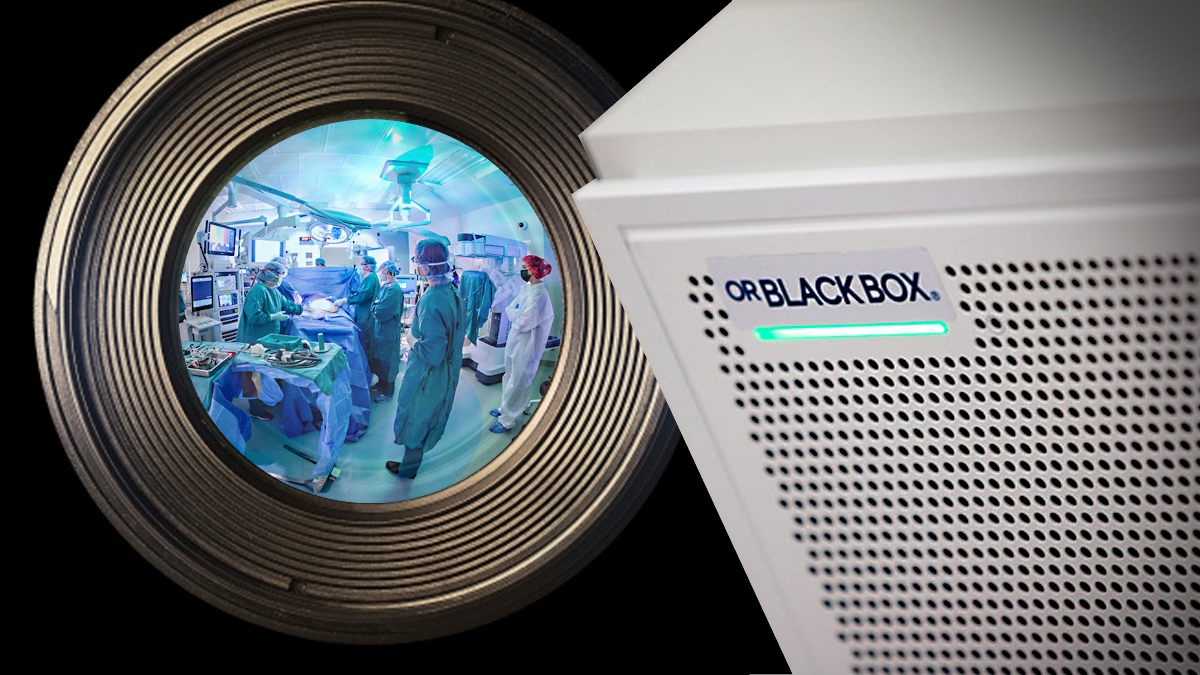
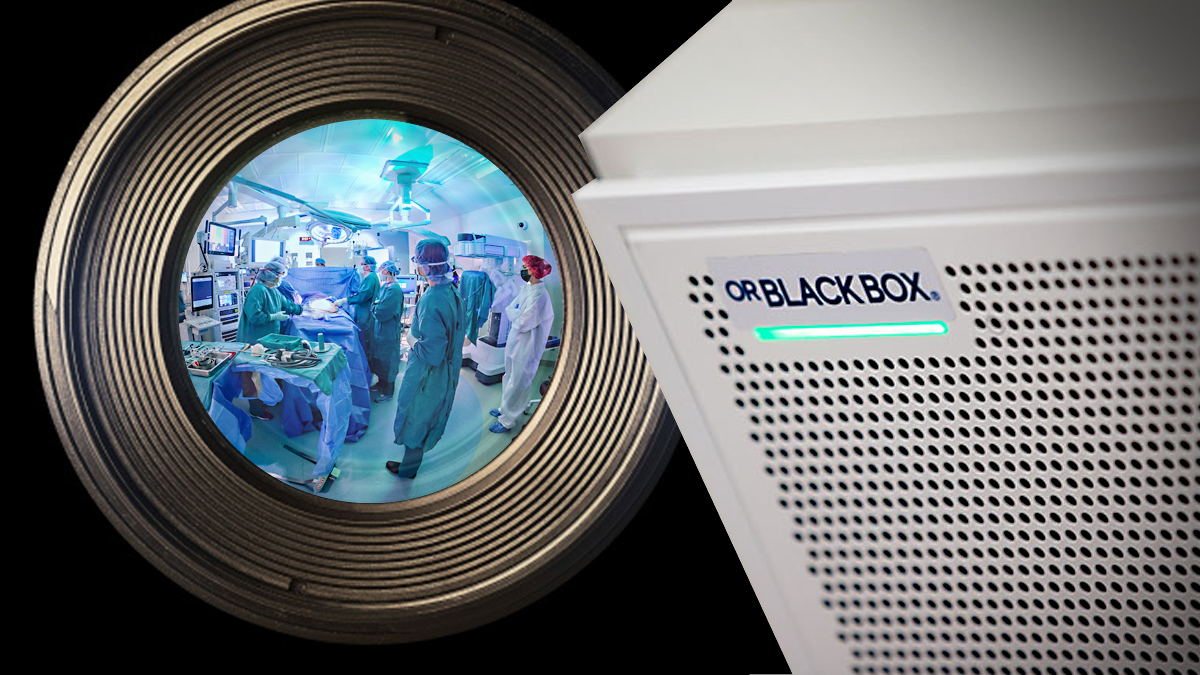
In 2006, after moving to the University of Toronto, he began working with a team of engineers, designers and researchers on a “black box” for the operating room (OR). The concept was fashioned after the black boxes found in aircraft that record flight data and cockpit conversations and allow airlines to improve safety by predicting and mitigating risks.
A few years later, the team installed the first prototype at a Toronto hospital.
Bringing 'Black Box' Technology to the OR
“I was inspired by aviation and what made aviation the safest form of transportation,” Grantcharov said in a Stanford Medicine report.
Today, the OR Black Box made by Surgical Safety Technologies Inc. in Toronto, which Grantcharov founded, is used in select ORs at Stanford Medicine and in a couple dozen hospitals in the U.S., Canada and Western Europe. The system comprises sensors and software and interacts with video, audio, patient vital signs and data captured from medical devices.
The technology is used primarily in ORs to analyze what goes on in the environment with the aim of improving systems to reduce medical errors and enhance safety and efficiency.
Enhancing Communications
Duke University Hospital is using black boxes in two ORs to study and improve patient positioning for surgery to reduce the possibility of skin and nerve injuries. The hospital also is exploring how the technology can be used to enhance communication among nurses during surgical procedures to see that key tasks are completed, such as confirming that surgical instruments and medical devices are ready for a procedure.
The technology also has helped Duke administrators find ways to improve systems for sending and tracking specimens, Rebecca McKenzie, assistant vice president for perioperative services, recently told The Wall Street Journal. The protocol for specimens, such as tissue removed and sent to a pathology lab, was revised to give clearer directions for each step in the process of handling a specimen and verify that it reaches the proper lab.
Teams also use information from the system to increase OR efficiency and productivity by reducing OR turnaround time.
Defining What Works
The University of Texas Southwestern Medical Center, which began using the OR Black Box in 2020, now uses five of the systems for a more detailed look at what practices characterize high-performing OR teams. Giving teams the ability to watch themselves provides powerful education and training opportunities, notes William Daniel, the medical center’s chief quality officer.
Although some clinicians initially were apprehensive about the possibility of the data being used for punitive purposes, they were reassured about how the data would be collected and used, giving way to acceptance as part of the hospital’s culture.
Mayo Clinic’s Rochester, Minnesota, facility has been working with the OR Black Box since 2021 and now uses it in three of its ORs to improve teamwork and identify ways to optimize the clinical environment.
The systems identified that some key pieces of equipment were taking too long to obtain at critical moments, Sean Cleary, M.D., a surgical oncologist at Mayo Clinic, recently told Becker’s Hospital Review. The solution: moving equipment closer to the working field to make it easier to access.
4 Things to Know about the OR Black Box
1 | It’s designed to help improve systems, not assign blame.
The system’s algorithms blur faces and bodies so that medical personnel can’t be identified. Aggregate data are deidentified and anonymized so users can learn from the information now and in the future, and audiovisual data is deleted after 30 days to protect confidentiality of patients and providers.
2 | It has many uses.
Duke University Hospitals plans to add more black boxes in the future and will prioritize robotic rooms while exploring uses in trauma bays and thoracic surgery.
3 | It blends with the OR environment.
The system is not a physical box but a system of sensors and data recorders. It was designed not to require human input and to work unobtrusively in the OR space.
4 | It provides an opportunity to enhance clinician dialogue.
Holding regular quality-improvement meetings can bring together OR professionals to review and discuss data obtained from the system.



