New Analysis Connects Better Outcomes
for Hospitalized Surgical Patients to
Improvements in Key Patient Safety Indicators
In September 2024, the American Hospital Association (AHA) published a report powered by Vizient® showing that hospital and health systems performed better on key patient safety and quality measures in early 2024 than they did before the COVID-19 pandemic. The report focused on the 22% reduction in risk of mortality for hospitalized patients in the first quarter of 2024 compared to the fourth quarter of 2019.
To gain deeper insight into the factors behind the reduced mortality risk, the AHA collaborated again with Vizient to conduct a more detailed analysis of data specific to hospitalized surgical patients. These follow-up analyses demonstrate not only a substantially lower risk of mortality for hospitalized surgical patients post-pandemic compared to pre-pandemic but also highlight several evidence-based factors that may have contributed to the improvement. Hospitals achieved substantial reductions in falls and certain infections – both of which also were shown to be improving in previous AHA Insights Reports – and reduced post-operative severe bleeding, sepsis and respiratory failure.
Hospitals also experienced significant increases in the average length of stay and acuity for surgical patients. These findings align with Vizient projections that more complex surgical patients are increasingly seeking care in hospitals, while those with less serious conditions are turning to outpatient settings. They also complement AHA analyses showing that tactics used by commercial insurers – particularly Medicare Advantage (MA) plans – are contributing to delayed discharges and denials of appropriate post-hospital care.
Hospitals and health systems remain committed to continually improving patient outcomes and advancing innovation in care for the patients and communities they serve.
Key Takeaways
- In the first quarter of 2024, hospitalized surgical patients were nearly 20% more likely to survive than expected — based on their underlying acuity — compared to patients in the fourth quarter of 2019.
- This significant improvement aligned not only with better performance on patient safety metrics — such as reductions in infections and falls — but also with marked declines in three high-risk complications strongly linked to mortality: post-operative hemorrhage, post-operative sepsis and post-operative respiratory failure.
- As an increasing number of surgical procedures are shifted to outpatient or ambulatory settings, the surgical patients who remain hospitalized tend to present with greater clinical complexity and require higher acuity care. Vizient projects that this trend will continue to intensify over the next decade.
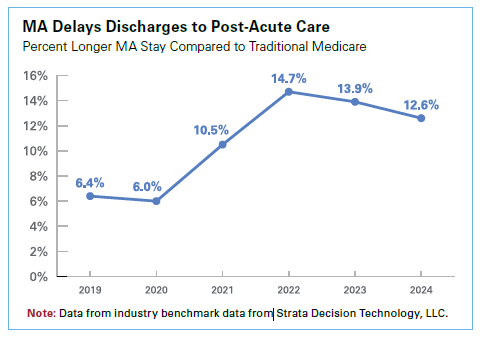
- The average length of stay for hospitalized surgical patients has increased by nearly one full day over the past five years. This rise correlates with both increasing patient acuity and a growing trend among insurers to delay discharges and deny coverage for appropriate post-acute care services.
About the Data
To produce this report, AHA partnered with Vizient, Inc., an independent, third-party, multi-faceted organization that supports hospitals and health systems in their efforts to deliver high quality care as efficiently as possible.
The Vizient Clinical Data Base contains information on more than 1,300 hospitals, submitted within 30 days of the end of each quarter. This provides real-time feedback to the participating hospitals and allows them to benchmark their performance against that of other general acute care hospitals. Data from the Vizient Clinical Data Base used by permission of Vizient, Inc. All rights reserved.
Vizient receives data on more than 14 million inpatients and 200 million outpatients annually. To analyze the trends from pre-pandemic through first quarter of 2024, Vizient identified a cohort of 713 general, acute care hospitals for which it had a complete 18 quarters of data from fourth quarter 2019 through first quarter 2024. These hospitals represent the wide spectrum of hospitals across 49 states and the District of Columbia, including the ranges outlined below. Of note, two hospitals analyzed in the original September 2024 cohort were not eligible for inclusion in this follow-up analysis limited only to hospitalized surgery patients.
| Comprehensive Academic Medical Center | 16% |
| Large, Specialized Complex Care Medical Center | 21% |
| Complex Care Medical Center | 23% |
| Community Hospital | 41% |
Studies have shown the continued rise in acuity for hospitalized surgery patients over the last two decades, and although surgical patients represented a smaller portion of overall patient days (36% based on 2023–2024 Vizient CDB data), Sg2 forecasts predict that future demand is expected to rise sharply among patients with more complex, high-acuity conditions*. Given the disproportionate weighting of care intensity toward surgical patients, Vizient used an MS-DRG-based delimiter to perform these analyses on a cohort specific to only hospitalized surgical patients.
See definitions for hospital types from Table 1, Vizient levels of inpatient acuity, and a more thorough description of the MS-DRG based surgery population in the appendix.
Risk of Mortality for Surgery Patients Is Decreasing
Risk-adjusted mortality rates are one way to assess how well hospitals are delivering safe and timely care. For many years, hospitals and public health officials have determined the success of efforts to reduce mortality by looking at the expected mortality rate of a patient population versus the actual mortality rate. Comparing actual mortality to expected mortality involves evaluating the actual number of deaths (observed) in hospitals against the number of deaths predicted based on models like those that the Centers for Medicare & Medicaid Services uses in its Value-based Purchasing program that account for multiple contributing factors (expected). When observed mortality is consistently lower than expected – e.g., when risk of mortality is less than 1 – it indicates that more people are surviving conditions that otherwise would be expected to be fatal, suggesting ongoing continuous improvement in patient care and treatment.
The analysis, which uses Vizient’s risk-adjustment methodology, shows that since 2022, hospital mortality rates have been better than expected and that the difference between expected and observed continues to grow. In the first quarter of 2024, risk of mortality in the Vizient analysis reached 0.79 or nearly 20% lower than its baseline of 0.97 in 2019.
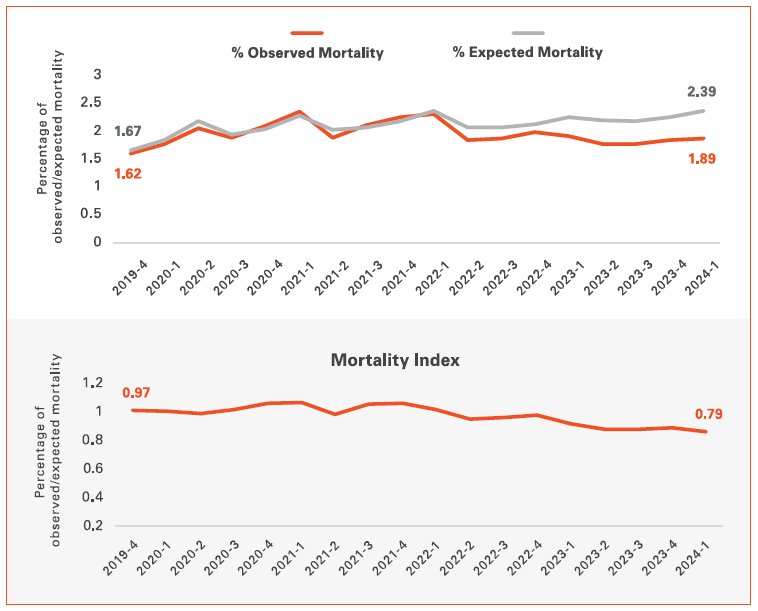
Source: Data from the Vizient Clinical Data Base used by permission of Vizient, Inc. All rights reserved.
Critical Surgical Patient Safety Indicators Are Improving
To better understand what could be contributing to this decrease in risk of mortality, Vizient analyzed performance across numerous patient safety indicators within the same cohort of hospitalized surgical patients. These indicators – which were originally created by the Agency for Healthcare Research and Quality and are tracked across various quality and patient safety measurement programs – include conditions that could substantially increase the risk of both major morbidity and death if they are experienced by surgical patients.
Three such indicators dramatically improved over the same period that overall risk of mortality decreased for hospitalized surgical patients. These included post-operative sepsis by 9.2%, post-operative respiratory failure by 19.0% and post-operative hemorrhage by 22.3%. Together, these reductions in patient safety indicators linked to mortality among surgical patients represent a key factor contributing to the overall improvement in survival rates for hospitalized surgical patients.
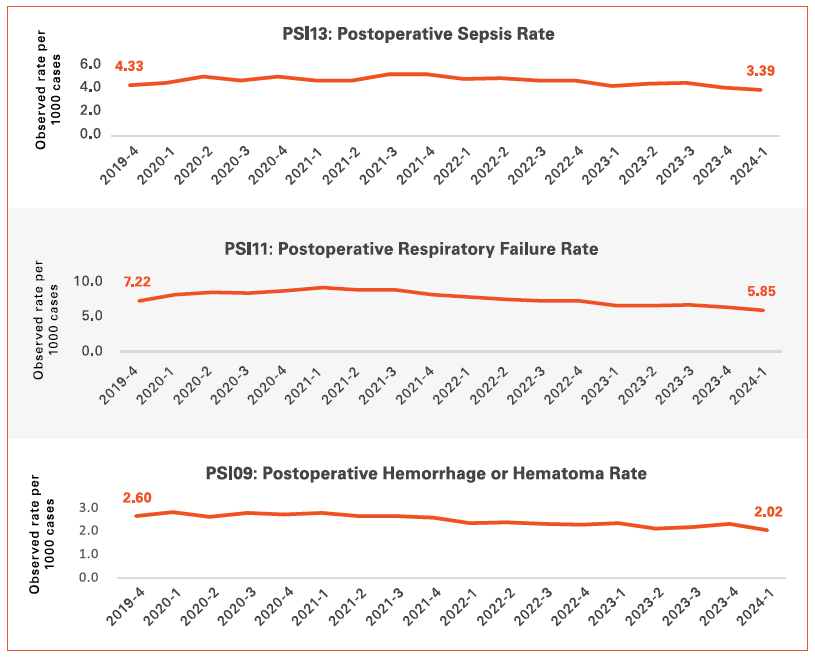
Source: CDB (4Q19-1Q24); Ages 18+; 2023 AMC Risk Model. MS-DRG Type: Surgical. Observed Rate per 1000 cases. Data from the Vizient Clinical Data Base used by permission of Vizient, Inc. All rights reserved.18+; 2023 AMC Risk Model. MS-DRG Type: Surgical. Observed Rate per 1000 cases. Data from the Vizient Clinical Data Base used by permission of Vizient, Inc. All rights reserved.
Infections and Falls Also Are Decreasing
Infections and falls among hospitalized surgical patients can significantly increase the risk of complications, prolong hospital stays and elevate the likelihood of mortality. As previously demonstrated in two recent AHA Insights Reports, as of the first quarter of 2024, hospitalized surgical patients are experiencing vascular catheter-associated infections (down 9.2%), catheter-associated urinary tract infections (down 6.6%) and falls (down 10.7%) at lower levels than those recorded in 2019. These improvements are likely contributing to the reduction in risk of mortality noted for hospitalized surgical patients.
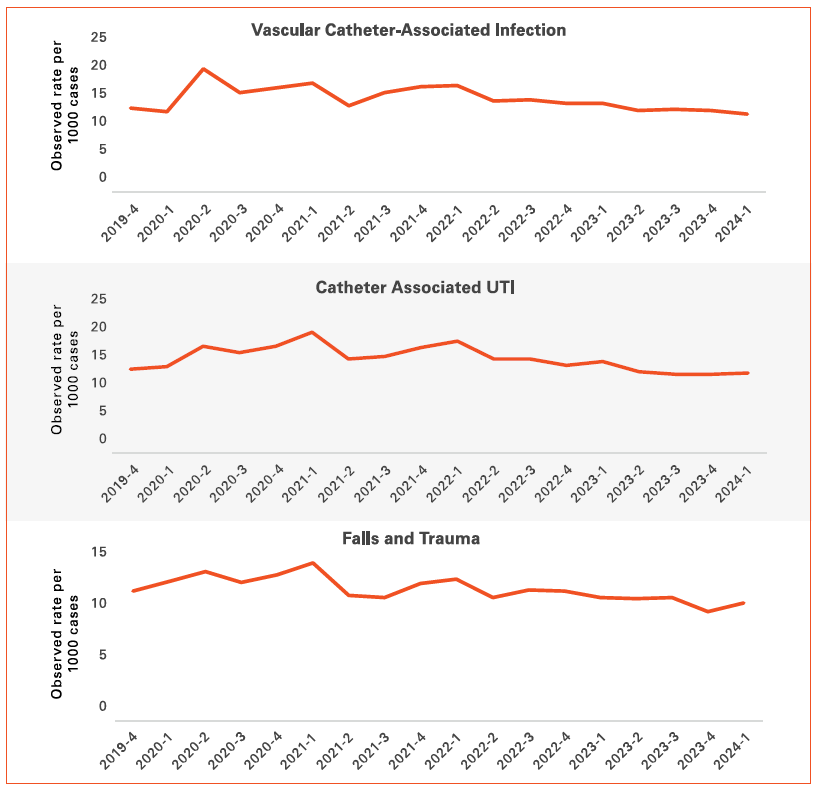
Source: CDB (4Q19-1Q24); Ages 18+; 2023 AMC Risk Model. MS-DRG Type: Surgical. Observed Rate per 1000 cases. Data from the Vizient Clinical Data Base used by permission of Vizient, Inc. All rights reserved.
Acuity for Hospitalized Surgery Patients Forecast to Continue Rising
As noted earlier, hospitals’ observed mortality rates decreased compared to what was expected, demonstrating substantial performance improvement. At the same time, the sharp rise in the expected death rate for hospitalized surgical patients shows that these patients are presenting sicker and need more complex care. Analysis by Sg2, a Vizient company, predicts that this trend will continue over the next 10 years. Despite comprising just 2% of 2025 hospital days, those who need the most intensive care, often called ‘quaternary’ patients, will drive the most days growth. By 2035, quaternary days are expected to grow 19%. Most of these very sick patients will be in the hospital for surgery.
Tertiary patient days — those with slightly lower care needs than quaternary patients but more than twice the complexity of lower-acuity patients — are projected to grow 16% by 2035, nearly all of the tertiary days are for surgical patients. Meanwhile, lower-acuity patient days (case mix index < 1.0), are expected to grow a modest 7% over the next decade, stemming mostly from medical patients.
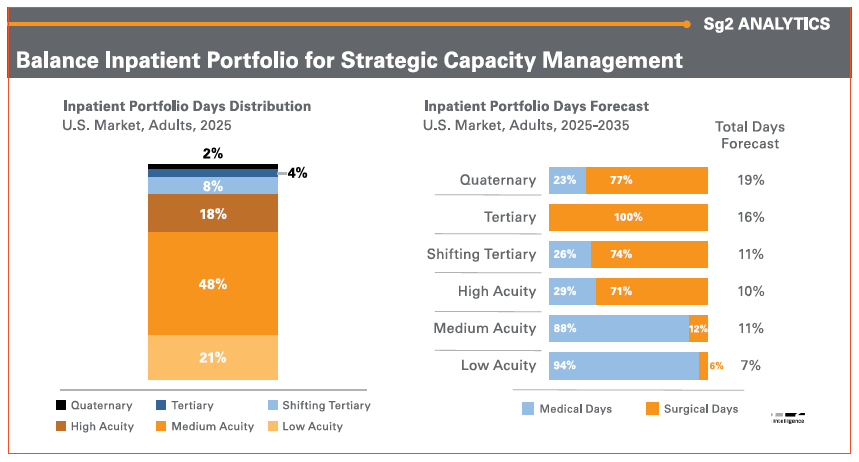
Note: Analysis excludes 0-17 age group. Percentages may not add to 100% due to rounding. Quaternary is Sg2 2025 Quaternary DRG list. Tertiary at risk shifting = DRGs removed from Sg2 Tertiary List from 2017 to 2025. High Acuity: CMS weighted DRGs > 2.0; Medium Acuity; CMS weighted DRGs 1.0 to 2.0; Low Acuity; CMS weighted DRGs < 1.0. Sources: Impact of Change®, 2025; HCUP National Inpatient Sample (NIS), Healthcare Cost Utilization Project (HCUP) 2021. Agency for Healthcare Research and Quality, Rockville, MD; Claritas Pop-Facts®, 2025; Sg2 Analysis, 2025.
Length of Stay Rising for Hospitalized Surgical Patients
The average hospital stay for surgical patients has increased by one full day compared to 2019. Despite improvements in several patient safety indicators – factors that are typically associated with shorter hospital stays – other elements appear to be contributing to the continued increase in length of stay. This includes a substantial rise in patient acuity and likely is also a result of delays in access to post-acute care placement by certain commercial insurance companies – particularly within the Medicare Advantage (MA) program.
Surgical patients who stay in the hospital often need continued care before returning home. This can include inpatient rehab or skilled nursing that help them recover. Delays in discharging patients to post-acute care are a growing problem for many patients and are a likely contributor to longer inpatient stays. These delays are often driven by prior authorization requirements or insufficient post-acute provider networks within MA plans. Among MA patients, the average length of stay prior to discharge to post-acute care has doubled relative to Traditional Medicare between 2019 and 2024, and further analyses can be found in the AHA’s Cost of Caring Report.
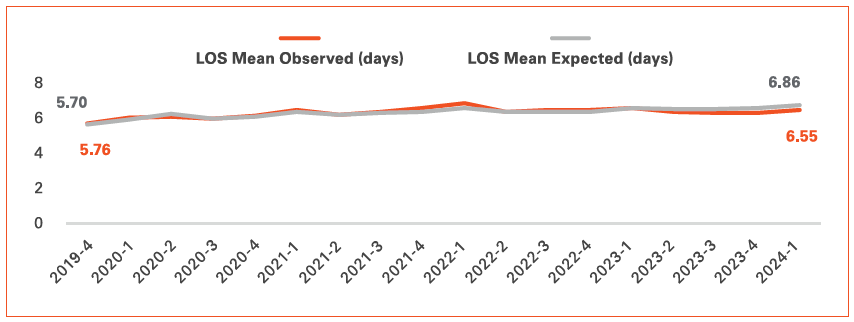
Source: Data from the Vizient Clinical Data Base used by permission of Vizient, Inc. All rights reserved.
Continuous Focus on Advancing Quality and Patient Safety
All hospitals and health systems strive to deliver safe, high-quality care to every patient they serve. The AHA’s Patient Safety Initiative, which was launched in 2023, is a collaborative, data-driven effort that helps hospitals and health systems work together to reinforce and accelerate patient safety efforts. The initiative provides hospitals with tools and data to advance patient safety, offers a platform for sharing their stories of improvement with peers, and highlights examples of applicable innovation that support, spread and sustain safety improvement. For more information, visit AHA’s Patient Safety Initiative webpage at aha.org/aha-patient-safety-initiative.
In collaboration with organizations like the AHA, Vizient is helping to shape a future where quality and safety are integral to every patient’s care journey. The Vizient Clinical Data Base provides patient outcomes data, collaborative benchmarking, evidence-based best practices that advance patient care and innovative tools to measure performance in real time. These data-driven insights support patient safety and care quality while also creating a culture of continuous learning and excellence for clinicians. Learn more about the Vizient Clinical Data Base.
Appendix: *Definitions of How Vizient Cohort Definitions
Comprehensive Academic Medical Center Criteria:
- At least 25 Solid Organ Transplants annually
- At least 600 Trauma Service line cases OR 1500 acute transfers in annually
- At least 125 combined cases Neurosurgery and Cardiothoracic Surgery annually
Large, Specialized Complex Care Medical Center Criteria:
- At least 25 solid organ transplants and 75 combined cardiothoracic and neurosurgery cases
- Or 600 trauma and 75 combined cardiothoracic and neurosurgery cases
- Or 1500 acute transfers in from another acute facility and 75 combined cardiothoracic and neurosurgery cases
Complex Care Medical Center Criteria:
- Not in the Comprehensive Academic Medical Center category or Large Specialized Complex Care category
- At least 25 combined cases Neurosurgery and Cardiothoracic Surgery annually
Community Hospital Criteria:
- Not in the previous described categories, excluding Critical Access & Specialty Hospitals
- Hospitals not included in the category criteria are critical access hospitals and specialty hospitals (cancer hospitals, children’s hospitals, other specialty hospitals).
* Based on Sg2 Impact of Change® 2025 Inpatient Portfolio Forecast, Adults, US Market 2025-2035



