The Burden of Violence to U.S. Hospitals
A Comprehensive Assessment of Financial Costs and Other Impacts of Workplace and Community Violence
Research Report - June 2, 2025
CONTENTS
KEY FINDINGS | EXECUTIVE SUMMARY | INTRODUCTION | FINANCIAL COSTS OF VIOLENCE | PRE-EVENT FINANCIAL COSTS | POST-EVENT FINANCIAL COSTS | OTHER IMPACTS OF VIOLENCE | LIMITATIONS | DISCUSSION
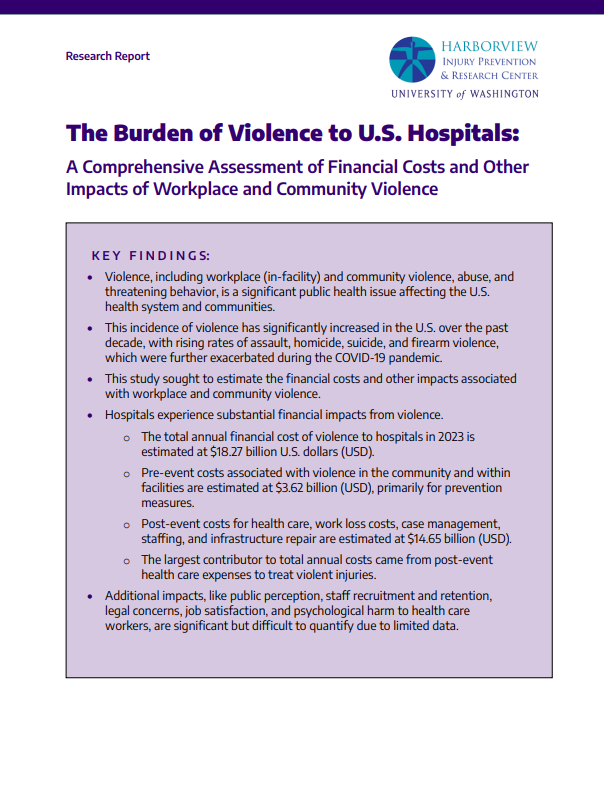
KEY FINDINGS:
- Violence, including workplace (in-facility) and community violence, abuse, and threatening behavior, is a significant public health issue affecting the U.S. health system and communities.
- This incidence of violence has significantly increased in the U.S. over the past decade, with rising rates of assault, homicide, suicide, and firearm violence, which were further exacerbated during the COVID-19 pandemic.
- This study sought to estimate the financial costs and other impacts associated with workplace and community violence.
- Hospitals experience substantial financial impacts from violence.
- The total annual financial cost of violence to hospitals in 2023 is estimated at $18.27 billion U.S. dollars (USD).
- Pre-event costs associated with violence in the community and within facilities are estimated at $3.62 billion (USD), primarily for prevention measures.
- Post-event costs for health care, work loss costs, case management, staffing, and infrastructure repair are estimated at $14.65 billion (USD).
- The largest contributor to total annual costs came from post-event health care expenses to treat violent injuries.
- Additional impacts, like public perception, staff recruitment and retention, legal concerns, job satisfaction, and psychological harm to health care workers, are significant but difficult to quantify due to limited data
EXECUTIVE SUMMARY
Violence is a major public health problem impacting our health system and communities.1 Over the past ten years, rates of violence have increased in the United States (U.S.), including rates of assault, homicide, suicide, and firearm violence.2–5 Further, violence increased during the COVID19 pandemic including rates of intimate partner violence, suicide, firearm violence, and workplace violence towards health care workers, and have not yet returned to pre-pandemic levels.6–10 Violence directly impacts hospitals via millions of emergency department visits and hospitalizations for fatal and nonfatal violence-related injuries each year.4,11 In addition, the impact of workplace and community violence is seen within the broader health care system leading to staff turnover, absenteeism, loss of productivity, high insurance and workers’ compensation costs, and an increased risk of depression, post-traumatic stress disorder, and suicide.12–15 The American Hospital Association (AHA) engaged the University of Washington (UW) Harborview Injury Prevention and Research Center (HIPRC) to estimate the financial costs and other impacts to hospitals from all types of violence, abuse, and threatening behavior within their facilities and communities. Through comprehensively characterizing the impacts of violence on hospitals, this report highlights the magnitude of violence as a public health problem and informs future policy and research efforts to address violence impacting U.S. hospitals and the health care system.
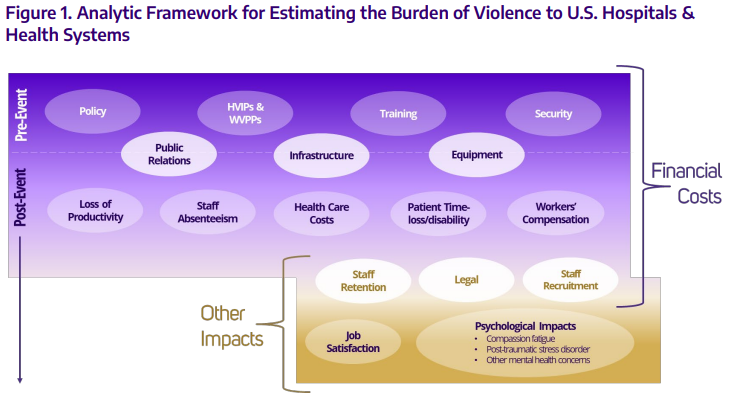
We used mixed methods that incorporated multiple data sources, including existing federal and state data sources, published literature, and primary data to quantify the impacts of violence on hospitals. Our estimates were guided by an analytic framework developed by the study team, experts in the field, and published literature. The framework incorporates financial costs and other impacts of violence, broken down by pre- and post-event costs. Beyond pre- and postevent costs, we analyzed financial cost estimates by violence type and examined other impacts resulting from violence, including staff satisfaction and productivity, staff retention and recruitment, psychological impacts, and legal and ethical concerns.
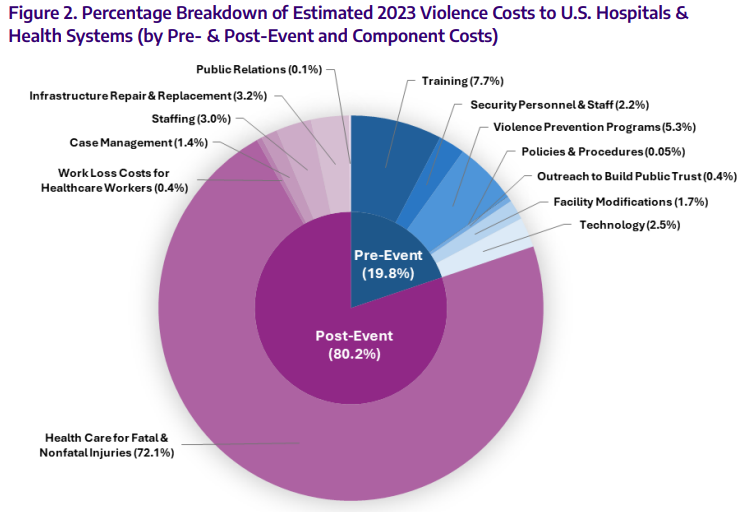
Overall, we estimate the total annual financial cost of violence to hospitals in 2023 to be $18.27 billion (U.S. dollars, USD). This estimate includes pre- and post-event cost components. Pre-event costs were estimated to be $3.62 billion (USD) and included costs for trainings, security and staffing, policy and procedure development, outreach to build public trust, facility modifications to prevent and mitigate harm, and investments in technology to monitor events. Post-event costs were estimated to be $14.65 billion (USD) and included costs for health care, staffing, replacement and repair of infrastructure and equipment, legal costs, and community and public relations costs. The largest contributor to total annual costs came from post-event health care expenses to treat violent injuries.
There are additional impacts of violence to hospitals that cannot be quantified at this time due to limited data availability. These far-reaching consequences include the impact of workplace violence on public perception, staff recruitment and retention, legal concerns impacting hospitals, job satisfaction for health care workers, and the psychological impacts on health care workers who experience or observe violence. These interconnected effects underscore the complex and pervasive nature of violence beyond immediately measurable costs to hospitals.
1. INTRODUCTION
1.1 BACKGROUND AND RATIONALE
Violence is a major public health problem impacting health systems in the United States (U.S.).1 In the past ten years, there has been an increase in the incidence of assault, homicide, suicide, and firearm violence in the U.S.2–5 Communities are highly impacted by violence, particularly in highpoverty and under-resourced neighborhoods.16–18 Additionally, the COVID-19 pandemic declared in March 2020 had direct impacts on increasing rates of intimate partner violence (IPV), suicide, firearm violence, and workplace violence (WPV) against health care workers.6–10 In 2022, there were 2,105,245 nonfatal and 73,989 fatal violence-related injuries that occurred in the U.S.11,19,20 Violence also occurs in hospitals, where health care workers experience significant rates of violence from patients and visitors.12,13 This leads to staff turnover, absenteeism, loss of productivity, high costs in disability and indemnity, and an increased risk of depression, posttraumatic stress disorder, and suicide.14,15
The American Hospital Association (AHA) engaged the University of Washington (UW) Harborview Injury Prevention and Research Center (HIPRC) to estimate the financial costs and other impacts to hospitals of all types of violence, abuse, and threatening behavior within their facilities and communities. The Human Subjects Review Committee at the UW Institutional Review Board approved this study (STUDY00019266; STUDY00019881). The goal of this report was to rigorously characterize and quantify the financial costs and other impacts of workplace and community violence to hospitals and their health systems, thus producing valuable information regarding the current impact of violence as a public health problem to inform policy and future research. We used mixed methods that incorporated multiple data sources to inform this report.
This report:
- Estimates the financial impact of violence to hospitals using published estimates, publicly available data sources, and primary data collection.
- Identifies other impacts of violence to hospitals using published estimates, publicly available data sources, and primary data collection.
- Identifies policy and research implications for addressing the impacts identified in the report.
1.2 ANALYTIC FRAMEWORK AND METHODS
For a more comprehensive review of the financial and other costs of violence, we used the World Health Organization’s definition of violence: “intentional use of physical force or power, threatened or actual, against oneself, another person, or against a group or community, which either results in or has a high likelihood of resulting in injury, death, psychological harm, maldevelopment or deprivation.” 21 Figure 1 below illustrates the analytic framework used to estimate the cost of violence to U.S. hospitals and health systems. This framework was developed by the study team and was guided by input from experts in the field and by review of current literature. The framework illustrates financial and other components used to derive our cost estimates, broken down by pre- and post-event costs. As illustrated in the framework, several components encompass both financial and other costs (i.e., Infrastructure and Equipment), and pre- and post-event costs (i.e., Staff Retention and Recruitment).
Mixed methods were used to estimate the financial costs and other impacts of violence to U.S. hospitals. We conducted a scoping review of the literature to ensure we captured a comprehensive overview of existing research, knowledge, and data related to the financial and other impacts of violence to U.S. hospitals. We included articles in our review that were published after 2016, focused on the U.S. health system, and published in English. Peer-reviewed studies and government reports were prioritized. Identified studies and extracted data were managed in Covidence online systematic review software. This review informed estimates reported here of the financial and other costs of violence and gaps in knowledge about cost components meriting future research.
We further used a socioecological framework to guide rigorous synthesis of existing literature, synthesis of recent national data describing direct and indirect costs in a diverse sample of care settings and health care workers (HCW), and in primary data collection to increase understanding of the true violence-related financial and operational pressures facing U.S. hospitals and their employees and patients.22 The scope of this report focuses on hospitals and their related health systems, heretofore referred to as “hospitals” unless otherwise indicated.
2. FINANCIAL COST OF VIOLENCE
Violence is a major public health problem in the U.S. As hospitals are directly impacted by workplace and community violence, understanding the financial costs to U.S. hospitals associated with violence is essential to guide cost-effective prevention efforts and to educate administrators, policymakers, and the public about the importance of prevention. Successful prevention relies on a comprehensive understanding of the many sides of a problem and designs complementary interventions from many angles; we have similarly structured our analysis of the financial cost of violence to hospitals to enable a comprehensive understanding of the many areas in which violence results in a financial cost, and the estimated magnitude of those costs. Although hospitals cannot address all workplace and community violence in the U.S., they are in a position to potentially have a significant impact on violence prevention in their facilities and surrounding communities.
| Cost Category | In millions of USD | Location of Violence | |
Community | Workplace | ||
| Pre-Event Financial Costs | 3,620.5 | ||
| Training costs | 1,403.7 | X | X |
| Security personnel and staffing | 404.3 | X | X |
| Violence prevention programs* | 959.2 | X | X |
| Policy and procedure development | 8.6 | X | X |
| Outreach to build public trust | 79.7 | X |
|
| Facility modification to prevent and mitigate harms | 306.0 | X |
|
| Investments in technology to monitor possible events | 459.0 | X | X |
| Post-Event Financial Costs | 14,648.8 | ||
| Health care costs for fatal and nonfatal injuries | 13,165.6 | X |
|
| Work loss costs for workers in the health care setting | 79.0 |
| X |
| Case management | 252.5 | X |
|
| Staffing | 541.3 | X | X |
| Replacement & repair of damaged infrastructure & equipment | 584.8 |
| X |
| Community interface and public relations | 25.6 | X | X |
| Note: Values may not sum to totals due to rounding. *Relates to expenses other than training | |||
Overall, we estimated the total financial cost of violence to hospitals to be $18.27 billion (U.S. Dollars, USD) (Table 1, Figure 2). This estimate includes pre- and post-event cost components. Pre-event costs were estimated to be $3.62 billion (USD) and included costs for trainings, security and staffing, prevention programs, policy and procedure development, outreach to build public trust, facility modifications to prevent and mitigate harm, and investments in technology to monitor events. Post-event costs were estimated to be $14.65 billion (USD) and included costs for health care, staffing, replacement and repair of infrastructure and equipment, and community and public relations costs. The largest contributor to total annual costs came from post-event health care expenses to treat violent injuries.
3. PRE-EVENT FINANCIAL COSTS
3.1 TRAINING COSTS
Preparation for violent events in the health care setting requires training of workers at each clinical location. The estimated costs associated with this pre-event violence-prevention training are summarized below. Training-related costs were divided into six categories of component costs corresponding to distinct types of training occurring within hospitals and health care facilities. Together, we estimated training costs at $1.4 billion annually, with most of the cost stemming from training staff on de-escalation, emergency preparedness, and institution-specific violence-related policies and procedures (Table 2). Activities in this section fall under several Joint Commission and Medicare Conditions of Participation Standards.23–35
| Cost Category | In millions of USD |
| Total training costs | 1,403.7 |
| Active shooter training | 61.7 |
| Training to respond to lateral violence | 148.0 |
| Training in emergency and medical surge preparedness | 369.5 |
| Training in de-escalation in hospitals | 377.4 |
| Training on violence-related policies and procedures in the hospital | 261.9 |
| Training for providers to identify violence-related trauma | 185.2 |
3.1.1 Active Shooter Training. Hospitals are not immune from experiencing WPV, including active shooter events. A study identified 88 hospital shootings in the U.S. from 2012 to 2016 noting emergency departments were the most common site (30%), followed by patient rooms (21%) and parking lots (15%). 36,37 Additional studies described perpetrators as those with a personal grudge against their victims and of 235 victims, at least 60-80% were bystanders to the violent event, 13% patients, 5% nursing staff, and 3% physicians. 36,38,39 Since most events transpire within 15 minutes, before law enforcement can arrive, the Joint Commission urges hospitals to prepare staff, particularly recommending the development of a communication plan, establishing processes and procedures to ensure patient and employee safety, training and drilling employees, and planning for post-event activities (e.g., establishing debriefing procedures). 40,41 Hospital training sessions often recommend the “Run-Hide-Fight” strategy and deliver other educational content through annual online modules or computer-based simulations.42,43 To estimate the cost of providing active shooter trainings in U.S. hospitals, we assumed that across all hospital employees, trainings employ a dual learning approach (online virtual e-learning as well as in-person sessions with trained instructors).44 We identified estimates from 2018 that indicate costs of blended types of training were approximately $32,100 (educational setting).45 In the absence of formal cost estimates for this type of training, we estimated that costs for this type of training vary by hospital size, wherein larger hospitals have higher costs due to having more staff. Assuming a starting annual cost of $6,000 for the smallest hospitals (6-24 beds) and increasing costs incrementally by 20% according to hospital bed size (8 tiers) to $21,499 for the largest hospitals, we estimated that all U.S. hospitals (N=6,120) pay approximately $61.7 million* annually for active shooter training, independent of other trainings described in this report. Activities in this section fall under several Joint Commission and Medicare Conditions of Participation Standards.23–29
3.1.2 Training to Respond to Lateral Workplace Violence. Stressors that arise in the hospital workplace, combined with hierarchy and behavioral norms, can create environments that enable lateral violence. Lateral violence is a type of workplace violence, defined as workplace conflict arising from interpersonal relations between employees. In the U.S., up to 76% of health care workers have reported experiencing violence, with over 80% experiencing verbal violence and 33% experiencing physical violence.46 Unfortunately, some of this violence is lateral violence arising from employees perpetrating abuse towards their colleagues via repeated behaviors of physical, psychological, or sexual abuse.47 There are a multitude of interventions available to decrease the prevalence of workplace incivility, lateral violence, and abuse and bullying.48
The Joint Commission Standard HR.01.05.03 requires that leadership, staff, and licensed practitioners participate in ongoing education and training in WPV; however, the content for each audience is determined by the hospital.49 Additionally, individual states’ requirements for sexual harassment training (one component of lateral/workplace violence) vary considerably.50,51 The length of training session and requirements can also vary by occupation.52,53 To account for this variation across hospitals, occupations, state requirements, and content, we assume that 60% of the hospital workforce engage in some sort of lateral violence prevention training annually. In the absence of data on duration of training across professions or occupations, we estimated that annual training lasts an average of one hour across all hospital occupations, an estimate that also accounts for the fact that this training may be bundled with other employee training (e.g., training on policies and procedures related to violence). To estimate the cost of training, we utilized workforce and wage data for occupations employed in hospitals (NAICS Sector 62-2000)54 (see Appendix).
Per these assumptions, we calculated costs as follows: ∑21i=1 𝐸𝑖 x 𝑊𝑖 x 𝑇𝑖 , wherein i is the index representing each type of occupation group (Appendix Table 1), Ei is the national employment estimate for the i th occupation, Wi is the estimated mean hourly wage per employee for the ith occupation, Pi is the percentage of institutions with lateral violence training annually (60%), and T is the time spent per year in training for the i th occupation (1 hr). Based on this approach, we estimated that training on WPV prevention (lateral violence) costs hospitals $148.0 million* annually. Activities in this section fall under several Joint Commission and Medicare Conditions of Participation Standards.23–29
3.1.3 Training in Emergency and Medical Surge Preparedness. Medical surge preparedness describes the ability of health care systems to manage a sudden influx of patients following unplanned, large-impact events, such as mass casualty incidents, natural disasters, or a pandemic. While not all these events may involve violence, training in medical surge preparedness is also necessary to respond to large-scale events that do involve violence (e.g., mass shootings, bombings). Estimating costs of training personnel in preparing for medical surges (or for emergency preparedness in general) vary widely across the literature.55 To estimate the costs of medical surge preparedness for U.S. hospitals, we estimated the average duration of the training as two hours per health care staff member per year, and two hours per protective services staff member per year. This estimate of duration is based on Department of Homeland Security Center for Domestic Preparedness Medical Surge Management course.56 We recognize the duration of training may vary by occupation. For cost estimations, we assumed a training session would take staff away from regular duties for those hours. The patient-facing hospital workforce was defined as health care practitioners and technical occupations (Standard Occupational Classification [SOC] 29-0000) and health care support occupations employed in hospitals (SOC 31-0000) (Appendix Table 1).54 The protective services workforce (SOC 33-0000), including security guards, was also included in this calculation. Assuming 2 hours of annual training for the occupations above, we estimated that hospitals spend a total of $369.5 million* on medical surge preparedness training each year. The cost of preparing and offering the training internally was not incorporated into this estimate; therefore, we believe this is likely a conservative estimate of the total (true) costs for this training. Activities in this section fall under several Joint Commission and Medicare Conditions of Participation Standards.23–29
3.1.4 Training in De-Escalation. De-escalation skills help mitigate the deleterious impacts of conflicts within the health care setting. De-escalation training is particularly common in the hospital setting and is listed as a requirement by the Joint Commission (HR.01.05.03).49 To calculate the national costs of de-escalation training for the patient-facing hospital workforce, the duration of training was estimated at an average of two hours per health care staff member per year and eight hours per protective services staff member per year.57–59 We recognize that the extent of annual training likely varies by clinical specialty and location. For cost estimations, we assumed a training session would take staff away from regular duties for the training time. The actual cost of the training was not incorporated because costs vary widely and many training sessions may be developed and offered internally by health care institutions for little/no cost; our estimate is likely conservative as some hospitals may engage outside agencies to provide this training for an additional cost. See Appendix Table 1 for details on patient-facing and protective services workforce in hospitals (SOC codes 29-0000, 31-0000, and 33-0000). Assuming two hours of annual de-escalation training for patient-facing occupations and eight hours of annual training for protective personnel, we estimated hospitals spend a total of $377.4 million† on deescalation training each year. Activities in this section fall under Joint Commission Standard HR.01.05.03 EP 29.26
3.1.5 Training on Violence-Related Policies and Procedures in Hospitals. Training on violence-related policies and procedures is critical to ensure that the health care workforce is prepared to respond to violence within U.S. hospitals and is required by accrediting bodies such as the Joint Commission and federal agencies such as the Centers for Medicare & Medicaid Services.49 Awareness of, and compliance with, policies help employees promote safety during violent events. Training covers zero-tolerance policies, reporting mechanisms, and appropriate staff roles and responsibilities in the event of a violent incident. The general policy/procedure training described here encompasses training on institution-specific policies and procedures and does not include specific training summarized elsewhere in the report (e.g., de-escalation training). We estimated the hospital management workforce (SOC 11-0000) engages in two hours of policy and procedure-related training related to violence prevention57–59 (e.g., monitoring, reporting, and investigating events) and all other hospital employees engage in 0.5 hours of training annually (e.g., how to report events). Based on these assumptions and wage and workforce estimates (Appendix Table 1, 21 occupations), the estimated cost of training specifically on violence-related policies and procedures in hospital was calculated as follows: ∑21i=1 𝐸𝑖 x 𝑊𝑖 x 𝑇𝑖 wherein i is the index representing each type of occupation group (see table below), Ei is the national employment estimate for the i th occupation, Wi is the estimated mean hourly wage per employee for the i th occupation, Ti is the number of hours spent per year in training for the i th occupation (described above). Based on this approach and 2023 mean hourly wage data reported by the Bureau of Labor Statistics, we estimated that training on violencerelated policies and procedures cost U.S. hospitals $261.9 million* annually. Activities in this section fall under several Joint Commission and Medicare Conditions of Participation Standards.23–28
3.1.6 Training for Providers to Identify Violence-Related Trauma. Educating hospital personnel to recognize trauma linked to violence is crucial for interrupting the cycle of violence and helping to ensure patients receive the care they need.60–62 Conditions of note include child and elder abuse, neglect, or maltreatment, and screening for self-harm/suicide, domestic violence, human trafficking, and intimate partner violence. We estimated that the patient-facing hospital workforce dedicates, on average, one hour annually for these trainings. This estimate of time commitment is based on mandated trainings for related conditions63 (e.g., 6 hours every 6 years for suicide prevention training in Washington State) with the assumption that each year, providers engage in at least one hour of training related to mandated reporting or child and elder abuse, neglect, or maltreatment, and screening for self-harm/suicide, domestic violence, and intimate partner violence. (This is likely an underestimate.) The patient-facing hospital workforce was defined as health care practitioners and technical occupations (SOC 29-0000) and health care support occupations employed in hospitals (SOC 31-0000). Additionally, we estimated four hours per year for human resources managers (SOC 11-3121) to organize and monitor the trainings and related compliance. Hourly wage estimates for 2023 were obtained from the Bureau of Labor Statistics.54 We used the following equation to calculate the total cost associated with training for providers to identify violence/violent injuries: (𝐻𝐻R × 𝑁𝐻R × 𝑊𝐻R) + (𝐻𝑃F × [(𝑁29 × 𝑊29) + (𝑁31 × 𝑊31)] wherein HHR is the hours per year human resources managers spend providing and monitoring trainings, HPF is the hours per year the patient-facing hospital workforce dedicate to this training, NHR is the estimated number of human resources managers, N29 and N31 are the estimated number of patient-facing providers (for each SOC group, 29-0000 and 31-0000, respectively), WHR is the estimated mean hourly wage of human resources managers, and W29 and W31 are the estimated mean hourly wage of each patient-facing provider group (see Appendix Table 1 for values). We estimated that each year, U.S. hospitals spend $185.2 million† to train patient-facing providers in recognition of abuse, risk for violence, and violence-related trauma. Activities in this section fall under several Medicare Conditions of Participation Standards.23–25
3.2. SECURITY PERSONNEL AND STAFFING
Hospitals employ security personnel to respond to incidents of violence and monitor the safety and security of the facility. Security personnel are trained to manage emergencies and work closely with health care teams to maintain a safe and secure environment. Their purpose is to prevent potential events by detecting/deterring threats while fostering a reassuring, safe environment. According to the Bureau of Labor Statistics, U.S. hospitals employed 49,280 security guards in 2023 (SOC code 33-9032). Annual mean wages for security guards in this setting is $45,080, equating to a total wage expenditure on security of $2,221,542,400. Based on previous work, assuming 18.2% of this cost is attributable to local crime rates, we estimated staffing security personnel in response to violence costs U.S. hospitals $404.3 million. 64*
3.3. VIOLENCE PREVENTION PROGRAMS
In recent years awareness of the importance of proactive action to prevent violence, and the role of hospitals in that prevention, has grown. This focus on prevention has taken two forms; one focused on patients and keeping them safe from further violent injury while addressing psychological sequela from their current injury, and one focused on keeping employees safe. Below we described these two types of programs and estimated their costs, totaling $959.2 million annually (Table 3). However, it is important to note that we were unable to estimate the potential cost-savings these programs may create by successfully preventing violent injury. It will be important in future work to include emerging evidence about the efficacy of these programs to prevent injuries to paint a full picture of the potential cost-effectiveness of the programs.
| Cost Category | In millions of USD |
|---|---|
| Violence prevention programs (expenses other than training) | 959.2 |
| Hospital-based violence intervention programs | 270.5 |
| Workplace violence prevention programs | 688.7 |
3.3.1 Hospital-based Violence Intervention Programs. There has been a growing awareness among health care providers that only treating physical wounds is insufficient to prevent downstream effects following victimization, and health care staff can and should do more to address the psychosocial needs of patients by integrating violence prevention into the delivery of health care. 65,66 Hospital-based Violence Intervention Programs (HVIPs) seek to mitigate and prevent recurrent violent injury (trauma recidivism) by identifying and offering victims of violent injury (stabbing, gunshot wounds, assault) a range of support services while in the trauma unit. 67 Following recovery or stabilization of the index injury, HVIPs then seek to link patients to community-based organizations and programs external to the hospital upon discharge with the goals of preventing the patient from experiencing a subsequent violent injury, breaking the cycle of violence, and addressing social needs. HVIPs are comprised of multidisciplinary teams including trauma surgeons, nurses, social workers, and other credible messengers. These programs operate from a trauma-informed perspective reflecting a “fundamental shift in thinking from the supposition that those who have experienced psychological trauma are either ‘sick’ or deficient in moral character to the notion that they are ‘injured’ and in need of healing”.67
A unique feature of HVIPs is that the team members approach patients at the bedside instead of waiting for patients to contact them for support. HVIP staff endeavor to engage victims of violent injury within the “golden hour”: the period in which victims of violent injury are most likely to agree to engage in services. HVIP staff are trained to engage patients of violent injury and build rapport with them. According to the 2022 AHA Annual Survey, an estimated 1,143 hospitals reported having violence prevention programs for the community. (This is likely an underestimate due to survey response rate; we also assume that more hospitals would have HVIP programs in 2023, given the increasing investment and interest in these programs. However, the most recent data are 2022, thus we relied on this estimate.) To estimate the costs of these programs borne by hospitals, we relied on estimates that HVIP programs cost approximately $10,798 per participant.68 Assuming that each hospital with a HVIP serves proportionally as many participants as the size of their hospital, we estimated that the smallest institutions (6-24 beds) serve two participants annually and midsize institutions (300-399 beds) serve 100 participants annually.68 The number of participants per hospital was thus scaled accordingly across 8 levels of hospital bed sizes (e.g., hospitals with 25-49 beds served an average of 20 participants; those with 400-499 beds served an average of 120 participants). Assuming each HVIP program will cost an average of $10,798 per participant (recognizing that the cost per participant in smaller hospitals will be higher than larger hospitals), we summed the products of overall HVIP cost per participant across all hospitals in the U.S (see equation below). These terms were used to calculate total cost as ∑ 𝐶𝐶 × 𝑃𝑃𝑛𝑛 × 𝑁𝑁𝑛𝑛 8 𝑛𝑛=1 wherein C is the average cost per participant, Pn is the number of participants per hospital scaled according to 8 levels of bed size (n) and Nn is the number of hospitals at least level of bed size. Nationally, the costs of staffing, transportation, crisis support, and operations for HVIP programs total to $901.8 million each year.68 Evidence suggests expenses for HVIPs are shared across hospitals, foundations, local communities, charities, philanthropy, and federal funding.69 Accordingly, we assumed that 30% of the costs of HVIP are the responsibility of the hospital, thus the total cost to hospitals for HVIPs annually is estimated at $270.5 million.* Our estimate exceeds previous per-hospital HVIP costs reported in the literature, and recent investments in community violence-prevention and inflation likely account for this difference.
3.3.2 Workplace Violence Prevention Programs. Programs to prevent WPV are becoming a standard practice in health care. Distinct from HVIPs, WPV prevention programs consist of strategies and policies implemented by institutions to prevent and manage violence in the workplace and foster a culture of safety.70 Key components of WPV prevention programs may involve risk assessment, reporting mechanisms, incident response plans, support services, and monitoring and evaluation. They can also include several component costs discussed elsewhere in this report, such as policy development and training and education (those costs are not duplicated here). The Joint Commission requires hospitals to have a WPV prevention program (LD.03.01.01 EP9)71 “led by a designated individual and developed and supported by a multidisciplinary team.”72 Multiple states also have requirements that hospitals have WPV prevention programs.73 Given these requirements, we assume that all U.S. hospitals have a violence prevention program. *
The cost of staffing time to lead and support hospital WPV prevention programs, including completing risk assessments, establishing and maintaining reporting mechanisms, developing and disseminating incident response plans, providing support services, and overseeing monitoring and evaluation, are not publicly available. As an estimate, we assume that one coordinator will lead the program (e.g., emergency management director, SOC code 11-9161, mean annual salary of $106,670).54 This individual is supported by a threat assessment team with representation from public safety, social work, physician administrators, and nursing administrators.74 This team reviews threat assessment protocol workups and identifies recurring issues, as well as discussing plans, programming, and program needs. We assume the threat assessment team will meet for one hour monthly. In addition, the WPV prevention coordinator is assumed to be supported by a collaborative WPV prevention committee, which will meet quarterly to discuss incidents, review data, and discuss trends, challenges, and root causes. The membership of this committee can include leadership from across the hospital.74 For this estimate, because not all hospitals have representation from all of these areas, we assume representation in the committee will include one chief executive, one medical/health services manager, a human resource manager, an emergency medicine physician, a behavioral health provider, an occupational health and safety specialist, and an operations specialties manager. This selection accounts for a wide range in member salaries (i.e., $32.65 to $192.26 per hour) in order to account for variation in hospital and committee structures across the U.S.74 We estimated staffing cost based on salary estimates from the Bureau of Labor Statistics for health care providers in hospitals (NAICS code 62-2000)75 (See Appendix Table 2). Overall, we estimated the average cost of staffing a WPV prevention program is $112,532 per hospital per year, totaling to $688.7 million† annually. Activities in this section fall under several Joint Commission and Medicare Conditions of Participation Standards.23–29
3.4 POLICY AND PROCEDURE DEVELOPMENT
An important aspect of prevention and response to violent events in hospitals is the development of facility-specific policies and procedures. This process involves the creation of comprehensive guidelines describing the steps to be taken before, during, and after a violent incident or event. Developing these policies and procedures includes the following tasks, which require time and effort by hospital leadership: conducting risk assessments to identify potential threats, developing reporting protocols, defining personnel roles and responsibilities, and establishing protocols for post-event support services (e.g., counseling).30 Effective policies and planning should involve regular training and drills (the costs of which are covered elsewhere in this report (e.g., training and violence prevention programs)). Estimates for initial policy development and revision are approximately $3,000-5,000. 76 After policies are in place, maintenance is approximately $1,000/year.77 We assume most hospitals in the U.S. have policies developed (90%) and are in the maintenance phase; 10% still require further policy/procedure development. Assuming policy and procedure development costs $5,000, the estimated annual hospital cost for policy and procedure development and maintenance is $8.6 million. * Activities in this section fall under several Joint Commission and Medicare Conditions of Participation Standards. 24,27,31–33
3.5. OUTREACH TO BUILD PUBLIC TRUST
Proactive engagement with the public through transparent communication, educational programs, and community partnerships helps to establish trust and credibility in the hospital and its status as a place of safety in the community. This process includes engagement with not only the surrounding communities, but also building strong relationships with law enforcement and community agencies.
To estimate these costs, we used cost data from nonprofit community hospitals as these hospitals annually report to the Internal Revenue Service (IRS) on the benefits they provide to their communities. From a review of 2020 tax filings, nonprofit community hospitals spent on average 0.1% of their total expenses on community building activities. 78 These community building activities could include university/school partnerships, engagements in community relations committees, environmental improvements, workforce and job development, violence prevention, childcare programs, and partnerships with local law enforcement agencies. A prior report by the AHA estimated 8.1% of community building activities were generally related to programs and activities directed to prevent violence in the community. 64
Using data from the 2022 AHA Annual survey, there are a total of 2,987 nonprofit community hospitals in the U.S. Given the total facility expense for these community hospitals ($984.2 billion), it is estimated that $984.2 million was spent on community building activities (assuming that the mean community investment of 0.1 percent holds across all hospitals). 79 Assuming that 8.1% of hospital expenses for community building and related activities, accounting for inflation from 2022 to 2023, we estimated that $79.7 million† dollars were spent on community building activities generally related to preventing violence. We excluded for-profit, psychiatric, long-term care, and federal government hospitals from this estimate given the lack of publicly available reporting on these expenditures. Thus, the actual amount hospitals spend on communitybuilding activities related to preventing violence is likely greater than estimated here.
3.6 FACILITY MODIFICATION TO PREVENT AND MITIGATE HARMS
Another pre-event cost component is the modification of hospital facilities to prevent violent events and mitigate harm. These costs may include structural changes such as redesigning floor plans to eliminate isolated areas and ensure clear lines of sight, reinforcing entry points, and creating designated safe areas. Additional components may include improving lighting and visibility in vulnerable areas, implementing secure access controls to restrict unauthorized entry, and modifying patient rooms and common areas (public spaces) to minimize the risk of weapon use. These facility-level physical modifications are important to creating a safe environment and ensuring that health care facilities are prepared to respond effectively to potential threats. 80 Facility modification engineering solutions include, for example, two exit routes for rooms and an alternative route for employees in case of an emergency. Providing areas for de-escalation and ensuring lighting is not harsh or causing undue glare is important. Barrier protection includes deep counters, lockable and secure bathrooms for staff members, and enclosed receptionist desks with bulletproof glass. While data on the costs of facility modification are not available, we estimated that facility modification associated specifically with the incorporation of violenceprevention modifications in the design would amount to a mean of 0.5% of a hospital’s reported capital expenditures. The 2022 AHA Annual Survey data reports a total of $61.2 billion in capital expenditures; thus, the estimated cost of incorporating violence-prevention facility modifications would be $306.0 million* per year for U.S. hospitals.
3.7. INVESTMENTS IN TECHNOLOGY TO MONITOR POSSIBLE EVENTS
In addition to modifications to physical facilities, hospitals and health systems must make investments in technology to predict and monitor possible events. 80,† Costs associated with technology investments are primarily comprised of maintaining and upgrading security systems, such as installing surveillance cameras, body-worn cameras, and alarm systems. Additional costs may be associated with installation of panic or duress alarms or similar equipment and communication devices, weapons detection technology and the cost associated in operating the technology, artificial intelligence to identify patients at high risk for violence, and information technology infrastructure to identify or predict risk of violence.82 Estimates of costs of individual technology approaches (e.g., metal detectors) are available; however, comprehensive data on the violence-prevention technology investments made by all hospitals in the U.S. are not available. Focusing solely on hospitals, where most violent events in the health care and social assistance industry occur, we estimate that ongoing technology expenses amount to 3% of hospital operating costs. ‡ We assumed an investment of 1% of reported hospital capital expenditures for half of hospitals for the expense of new violence-prevention technology installment annually. 83 Additionally, we assumed that hospitals dedicate an additional 0.5% for maintenance of this technology. This amounts to $459.0 million* per year for U.S. hospitals. Activities in this section fall under multiple Joint Commission Standards.34,35
4. POST-EVENT FINANCIAL COSTS
This section outlines financial costs incurred following a violent event. Beyond the specific component costs detailed below, a hospital’s ability to provide patient care may be compromised immediately or shortly after such an incident. This disruption can result in unmet patient needs and a potential loss of revenue for the hospital. Although challenging to quantify, this impact should be considered in conjunction with the other costs discussed in this section.
4.1 HEALTH CARE COSTS FOR FATAL AND NONFATAL INJURIES
Total health care costs associated with violence borne by the hospitals were generated as the sum of the following components: costs from uninsured injuries and costs due to underpayments for patients with public insurance† . We estimated 23.6% of violence-related injuries treated in hospitals and emergency departments were among uninsured patients and thus hospitals would be uncompensated for this percentage.84 This estimate is consistent with recent national estimates of violence-related emergency department visits and hospitalizations. 85
In addition to violence-related costs borne by the hospital resulting from uninsurance, underpayments associated with set payment schedules for public insurers also generate costs borne by the hospital, rather than the patient or payer. We estimated a 12%86, ‡ underpayment rate for Medicaid and an 18%87,§ underpayment rate for Medicare, based on reporting from the AHA. We recognize these estimates are somewhat dated (2020 for Medicaid and 2022 for Medicare); however, they are the most recent data available from a reliable source. We estimated 39.8% of victims of violence were insured by Medicaid and 7.8% were insured by Medicare. 84
For health care cost estimates for treat-and-release emergency department visits, nonfatal hospitalizations, and fatal injuries due to violence, we relied upon estimates from the Centers for Disease Control and Prevention (CDC) Web-based Injury Statistics Query and Reporting System (WISQARS). Methodologies used to generate WISQARS estimates are reported elsewhere.88 Briefly, the total health care costs are based on statistical modelling of observed injury-related medical cost data; fatal injury medical cost estimates include treatment costs as well as coroner/medical examiner costs and costs associated with ambulance transport, nursing home care, or hospice care.88 Because the coroner and medical examiner costs are typically the responsibility of the patient’s family and not covered, for example, by public insurance, we excluded coroner/medical examiner costs from our estimates. It is expected that all violencerelated deaths should involve coroner/medical examiner services and the average estimated cost per exam was $3,000, which is a conservative 2018 estimate based on the U.S. Bureau of Justice Statistics reporting; the cost is likely higher now.89 The estimated medical examiner/coroner amount was removed from the calculations.
The estimates for costs and total number of fatalities due to violence are derived from CDC WISQARS, which generates 2021 USD estimates. These values were adjusted for inflation to 2023 USD using the Bureau of Economic Analysis Index annual change estimate (for health).90,*
Based on these data and assumptions, total health care cost borne by U.S. hospitals was estimated using the equation below (variable definitions and sources in Appendix Table 3). 1 × {[𝐶hospital + 𝐶𝐸D + (𝐶fatal − (𝐶examiner))] × [(𝑚 × 𝑢𝑚) + (𝑐 × 𝑢𝑐) + (𝑛 × 𝑢𝑛)]} Using this approach, the total estimated health care costs borne by hospitals for fatal and nonfatal injuries is $13.2 billion† in 2023 USD. This estimate represents only the costs for which the hospital is responsible due to un/under-reimbursed care and comprises 29.8% of the total estimated treatment costs for violence-related injuries in 2023 ($44.2 billion, Chospital + CED + Cfatal as reported by CDC WISQARS and adjusted for inflation to 2023 USD).
We also calculated costs associated with medical care for violence-related injuries for three types of violent injuries: cut/pierce, struck by/against, and firearm-related injury. Cut and pierce injuries involve an incision, slash, perforation, or puncture by a pointed or sharp instrument, weapon, or object (e.g., stabbings).91 Injuries classified as “struck by/against” involve a strike by or against an object or other person.92 The costs associated with these injuries which contribute to the total estimate of $13.2 billion are $4.1 billion for struck by/against injuries, $3.3 billion for firearm injuries, and $2.5 billion for cut/pierce/stab injuries. (Other injuries could be attributed to falls, inhalation, ingestion, suffocation, poisoning, or other causes.)
4.2 WORK LOSS COSTS FOR HOSPITAL WORKERS
The health care field accounts for approximately three-quarters of all nonfatal violence-related occupational injuries and illnesses in the U.S.93 The total cost to hospitals associated with time away from work for violence-related injuries among health care workers was estimated based on the Bureau of Labor Statistics data for the U.S. health care workforce.94 In 2022, an estimated 16,990 workers in hospitals had a violence-related nonfatal occupational injury or illness that involved days away from work. Another 8,740 hospital workers had days of restricted work activity or job transfer due to violence-related occupational injury or illness.
Across all industries, occupational injuries or illnesses from intentional injury resulted in a median of 7 days away from work. The distribution of days away from work is as follows: 1 day – 14.9%, 2 days – 11.9%, 3-5 days – 19.4%, 6-10 days – 12.9%, 11-20 days – 11.4%, 21-30 days – 6.4%, 31 or more days – 23.1%.94 Assuming that time loss within the health care field due to these injuries is similar to time loss across all industries and 2022 rates are similar to 2023, we estimated the costs of missed work based on the mean hourly salary for workers in hospitals: ∑7i=1 (𝑤 × ℎ × 𝐷𝑖 × 𝐼 × 𝑃𝑖), wherein w is the mean hourly wage for workers in the health care and social services fields, h represents the assumed number of hours in a workday, Di is the days missed at the ith interval, I is the number of violence-related occupational injuries, Pi is the percentage of workers reported above at the ith interval. For the days away from work with ranges, we used the highcentral digit (e.g., for 21-30, we used 25 days). Together, this sums to $52.7 million* in costs associated with time away from work due to violence-related occupational injuries and illnesses within the health care field. This estimate includes the entire workforce, including security guards.
As noted above, 8,740 hospital workers had days of restricted work activity or job transfer due to violence-related occupational injury or illness. No published estimate exists of the cost of changes in jobs or transfer due to violence-related occupational illness or injury. For this analysis, we are assuming a minimum cost of $3,000 per employee required to restrict work activity or transfer jobs (including vocational rehabilitation) due to violence-related occupational injury or illness.95,96 This estimate is thought to account for the wide range of possible restrictions and the cost of retraining employees and amounts to a total of $26.2 million.†
Together, we estimated work loss costs for the hospital workforce injured due to violence and missing at least one day of work is $79.0 million‡ per year. This is likely to be an underestimate and does not account for reduced productivity or time loss due to untreated elements of injury, such as psychological harm, work missed due to post-traumatic stress disorder (PTSD), or unreported injuries. The experience of violence is common in the hospital workplace and underreporting frequently occurs for myriad reasons.97
4.3 CASE MANAGEMENT
Case managers are unique health care professionals who work directly with patients to provide personalized support and guidance, including connecting to community resources and coordinating care and services. By efficiently coordinating care, case management is associated with improved outcomes, shorter lengths of stay, and lower readmissions rates. By overseeing the care of patients with violence-related injuries, hospitals can also optimize the use of resources. Previous work estimated that utilization management accounted for 2.1% of all patient care costs for hospitalized patients.64 Based on an annual estimate of 1.43 million nonfatal hospitalizations due to violence-related injuries amounting to $12.0 billion (inflation-adjusted from CDC WISQARS estimate to 2023 USD),90 this equates to a national inflation-adjusted hospital cost of $252.5 million.98
4.4 STAFFING
Violence in the workplace impacts workers beyond injuries and illnesses. WPV can be associated with employee absenteeism, loss of productivity, and turnover. Each of these component costs is summarized below. Together, these costs equate to an estimated $541.3 million annually (Table 4).
| Cost Category | In millions of USD |
|---|---|
| Staffing | 541.3 |
| Absenteeism | 139.2 |
| Loss of productivity | 183.8 |
| Turnover | 218.3 |
4.4.1 Employee Absenteeism. Exposure to violent incidents can lead to not only physical injuries, but also emotional trauma, heightened levels of stress, reduced morale, and burnout. These effects may contribute to an increase in employee absenteeism. Costs associated with employee absenteeism include increased expenditures on temporary staffing or overtime to account for absent workers and potential loss of revenue. Absenteeism associated with time loss for an occupational injury or illness was discussed earlier; this estimate focuses on health care worker absenteeism resulting from exposure to violence within the workplace or in the community, including within their own circle (e.g., IPV). This absenteeism can take place in the form of sick days or unpaid days, both of which impact the health care system. Estimates of absenteeism for victims of violence range from 5 to 25 days.99 According to the Bureau of Justice Statistics at the U.S. Department of Justice, the rate of violent victimization (including rape, sexual assault, robbery, aggravated assault, or simple assault) was 23.5 victimizations per 1,000 persons in 2022.100 Specific occupations, such as patient-facing occupations (e.g., health care practitioners or health care support occupations) face higher rates of exposure to violent events. For this estimate, we assumed a 2.35% WPV exposure rate for most occupations in hospitals.100 For patient-facing occupations and security/protective services occupations, we assume an exposure rate of 62%.101
Based on an estimated 6.2 million people working in hospitals in the U.S. and WPV exposures rates noted above, we estimated 146,515 hospital workers may be exposed to/victims of violence each year. Assuming that among those who experience violence, approximately 15% have 8 hours (1 day) missed from work annually.102 This is a conservative assumption: some research suggests up to 5 days.102 We estimated that the cost of absenteeism due to violence is $139.2 million.*
4.4.2 Employee Loss of Productivity. A frequent outcome of exposure to violence is loss of productivity in the workplace, which can be characterized by poor decision-making and attitude, disengagement, and overall low morale. In the health care setting, this can also result in poor patient outcomes. Costs associated with loss of productivity include the need to increase staffing to account for loss of revenue. Given the complexities of occupations and job tasks within hospital settings, loss of productivity is challenging to estimate. Among the estimated 2.8 million hospital workers estimated to experience violence annually, we conservatively assume one in twenty experience a reduction in productivity of 3% on average (approximately 60 hours per year for a full-time worker). Based on estimated annual salaries specific to each occupation and anticipated exposure to violence (varying by occupation time), we estimated that costs due to lost productivity amount to $183.8 million† annually.
4.4.3 Employee Turnover. Similar to employee absenteeism and loss of productivity, the physical and psychological toll of exposure to violence in hospital employees can contribute to high absenteeism rates, which can in turn strain remaining staff. Increased staff burden can lead to further burnout and turnover, ultimately impacting the quality of patient care and overall operational efficiency of the health care facility.‡ Research reveals that exposure to WPV impacts turnover intention among health care providers.103 This is only one factor contributing to turnover, and it is challenging to estimate the sole impact of violence in the workplace or community on health care professional turnover, despite recognizing that this extrinsic influence exists and contributes to decision-making. We calculated the estimated turnover rate for employees in the health care sector as the average monthly total separation104 divided by the average monthly employment.105 For 2023, the turnover rate was calculated as 3.31% (712,250 ÷ 21,525,325). This estimate was used for all workers except health care practitioners and technical occupations (SOC code 29-0000) and health care support occupations (SOC code 31-0000), which tend to have higher rates of turnover. For these occupations, we assumed a turnover rate of 5%106 which is likely an underestimate given that home health and nursing home employees have higher turnover rates.107,108 Based on these turnover rates, we estimated 1.1 million people working in the health care and social assistance fields in the U.S. will leave their jobs annually. We assume that a small percentage of these are associated with violence (1.5% based on previous research and increases in the incidence of violence over time)109 for all occupations other than health care practitioners and technical occupations, health care support occupations, and protective services occupations (SOC code 33-0000), which we assumed had a higher rate of violence exposure and thus a higher contribution of violence to turnover (3.0%). On average, the cost of turnover in health care equates to approximately 6-9 months’ worth of workers’ salaries.110 Using occupationspecific mean estimates of monthly salaries,111 this would equate to a range of costs from $174.7 million to $262.0 million (using 6- and 9-month salaries as cost multipliers, respectively), averaging to $218.3 million* annually.111 This estimate relates specifically to turnover among hospital employees exposed to in-facility or community violence.
4.5 REPLACEMENT AND REPAIR OF INFRASTRUCTURE AND EQUIPMENT
Violent events and incidents result in damage to hospital/health care facility infrastructure and equipment (i.e. security equipment, walls, furniture, medical equipment, and supplies), requiring their replacement or repair.112 Estimates of the actual costs of damage to infrastructure are not available. However, research has shown that rates of violent crime increase in proportion to population size.113 Assuming this pattern extends to hospital facilities within communities, we estimated that damage to hospital infrastructure varies by location. Specifically, we project that metropolitan hospitals (n=4,231) experience proportionally more damage than micropolitan (n=859) or rural (n=1,103) hospitals (values based on 2022 AHA Annual Survey estimates). We estimated that each year, metropolitan hospitals are responsible for replacement and repair of infrastructure and equipment equating to 1% of their reported capital expenses. We estimated that micropolitan and rural hospitals are responsible for 0.5% and 0.25%, respectively, of their capital expenses for repairs and replacements resulting from violence within the facility and surrounding community.† Accounting for this differentiation across hospitals, we estimated that the annual cost of replacement and repair of infrastructure and equipment due to violence is $564.6 million in metropolitan hospitals, $16.8 million in micropolitan hospitals, and $3.5 million in rural hospitals, equating to a total cost of $584.8 million. ‡
4.6 COMMUNITY INTERFACE AND PUBLIC RELATIONS
Hospitals, as pillars of their communities, have a public health responsibility to address violent events that occur within and outside health care facilities. This may include post-event debriefing, public health communications, relationship building with communities, and media relations. Public relations managers and specialists at hospitals play key roles in these duties. In 2023, there were 1,340 public relations managers and 4,290 public relation specialists working with hospitals, with average annual salaries of $141,820 and $75,000 dollars, respectively. 114 Assuming 5% of public relations managers’ and specialists’ time is spent on duties relating to post-violent event public relations,115,116 the cost to hospitals for community interface and public relations due to violence was $25.6 million§ dollars.
In addition to public relations managers’ and specialists' time spent on community interface and public relations addressing violent events, there are also costs attributed to materials (i.e., print and digital materials), equipment, and infrastructure for these public relations. These hospital costs are incorporated in the other cost estimates above.
5. OTHER IMPACTS OF VIOLENCE
Data limitations restricted our ability to provide financial estimates for all identified areas in which violence affects U.S. hospitals and health care workers using the comprehensive definition of violence provided above. Most importantly, we were not able to quantify financially the full toll of violence on the psychological and emotional health of workers beyond the outcomes of absenteeism, productivity, and staff turnover. The presence of such broader mental health effects are apparent in a multitude of studies documenting correlations in exposure to violence and various mental health and workplace satisfaction outcomes in workers. In lieu of providing financial estimates for the following components, we describe more comprehensively the incidence of workplace violence in different settings to provide the best available understanding of the magnitude of exposure in health care workers. We then provide summaries of data currently available describing associations between exposure to violence, mental health, and employee satisfaction in U.S. health care settings. While we were not able to generate reliable comprehensive financial estimates of associated costs for these components, an understanding of the incidence of exposure to violence and data on related mental health outcomes yields valuable insight and comprises an essential part of a comprehensive evaluation of the true burden of violence to U.S. hospitals and hospital workers.
5.1 INCIDENCE OF WORKPLACE VIOLENCE
In hospitals, WPV most often occurs in psychiatric departments, emergency departments (ED), waiting rooms, and geriatric units, with rural areas having higher prevalence rates than urban areas.117,118 However, HCWs from across different geographic and clinical locations, specialties, and roles can all experience WPV. One estimate suggests WPV prevalence ranges from 24.4% to 59.3% for physicians, 9.5% to 62.1% for nurses, 15.1% to 68.4% for receptionists, and 24.5% to 40.0% for technicians.118 Prevalence rates ranged from 14.0% to 57.4% for threats, 2.5% to 5.7% for bullying, 0.5% to 15.9% for physical assault, and 0.2% to 9.3% for sexual assault and harassment for HCWs in this study.118 Registered nurses (RNs), nursing assistants, and patient care assistants experience particularly high rates of WPV.119–121 At a South Florida community hospital, certified nursing assistants were found to experience the highest rates of workplace incivility compared to RNs and other clinical and non-clinical staff.119 According to a 2024 report, half of U.S. nurses have reported being either verbally abused, physically assaulted, or both by a patient or a patient’s family member within the previous two years.122 More than one in four of these nurses reported being likely to leave their positions as a result.122 Additionally, among 9,150 RNs in Michigan surveyed in 2022 regarding WPV concerns, 43% reported emotional abuse, 26% reported workplace bullying, 22% reported physical abuse, and 10% reported sexual abuse in the past 12 months.120 In another study that surveyed 138 RNs and patient care assistants, respondents experienced higher rates of verbal aggression than physical aggression by both patients and staff.121
Medical residents, nurses in training, and other health care trainees are also impacted by WPV. Out of 119 emergency medicine residents in New York state, 66% reported experiencing at least one act of physical violence during an ED shift. Of that sample, 97% experienced verbal harassment, 78% endorsed verbal threats, and 52% reported sexual harassment.123 Female medical residents and nursing trainees experience higher rates of sexual harassment and nonphysical WPV than their male counterparts.124,125 Out of 195 junior- and senior-level nursing students in the midwestern U.S., 82.6% had experienced verbal aggression, 60.5% experienced sexual harassment, and 52.3% experienced physical violence at some point during their training.125 These experiences can lead individuals to question their decision to join the health care workforce and negatively impact their psychological well-being.126–128 In fact, among 7,409 general surgical residents from 262 different general surgical residency programs, 30.2% had experienced verbal abuse, 38.5% reported experiencing burnout symptoms at least once a week, and 4.5% endorsed having suicidal thoughts in the past year.127
5.2 PSYCHOLOGICAL AND EMOTIONAL IMPACT OF VIOLENCE
Witnessing or experiencing violence in the hospital can lead to short and long-term psychological and emotional effects, including compassion fatigue, PTSD, and other mental health concerns, in addition to general satisfaction with one’s job. (We describe below compassion fatigue and PTSD, while acknowledging that the mental health impacts of exposure to violence may extend beyond these conditions.)
5.2.1 Compassion Fatigue. Compassion fatigue occurs when HCWs experience burnout and secondary traumatic stress and can result in low job satisfaction and emotional detachment from one’s work.129 Frequent exposure to WPV has been found to increase levels of burnout among HCW. Burnout adversely impacts workers’ physical and mental well-being, and often impairs their ability to effectively carry out workplace duties.130,131 Secondary traumatic stress is a stress response to hearing or witnessing the traumatic experience of another. The symptoms mimic that of PTSD and are intricately connected with those of burnout.132 In fact, high levels of distress, compassion fatigue, and low perceived institutional support have contributed to higher levels of stress among HCWs who experience mistreatment from patients.133
5.2.2 Post-Traumatic Stress Disorder. According to Hou (2024), experiencing violence in any form can lead to the development of PTSD, characterized by sleep disturbances, irritability, difficulty concentrating, feelings of frustration and powerlessness, intrusive recollections of the traumatic event, and emotional distress.134 Among 132 ED staff surveyed in McGuire et al., 21.3% respondents had experienced symptoms of PTSD due to WPV, and 18.5% reported considering leaving their position as a result.135 Similarly, Konttila et al. reported that psychiatric nursing staff who were repeatedly exposed to various forms of violence, including sexual attacks, non-verbal intimidation, and verbal threats, experienced significantly increased psychological distress and fear.136
5.2.3 Employee Satisfaction. In addition to the psychological, emotional, and physical impacts of exposure to violence, HCWs also experience reduced job satisfaction.137–140 For example, HCWs can experience a decreased desire to interact with patients and their families after experiencing WPV.137 This effect was found to be more pronounced among those working in an inpatient versus outpatient setting.137 ED nurses, in particular, have reported that continuous exposure to aggressive patients has negatively impacted their attitudes about their profession, affecting their ability to care for and desire to interact with patients.138,140,141 Lateral violence between health care worker colleagues also contributes to job dissatisfaction.119,141,142 Out of 91 ED attending physicians, residents, and mid-level providers in Detroit, 22.2% reported a specific instance of lateral violence in the preceding 12 months that negatively impacted their ability to provide care for their patients.142 Over 10% reported that lateral violence affected their personal health, led them to consider quitting their job, made them feel unsafe at work, or caused them to dread going to work due to fear of bullying.142
5.3 LEGAL AND ETHICAL CONCERNS
5.3.1 Legal Costs. Costs related to abuse or violence within hospitals, such as patient abuse, legal expenses for addressing community violence, and regulatory compliance issues are significant. However, comprehensive data on legal costs and citations are not publicly available.
5.3.2 Reporting Workplace Violence. Underreporting WPV remains a significant barrier for understanding its true prevalence.118,134,135,138,143,144 A common reason HCWs do not report WPV is due to unclear and unstandardized reporting channels.118,145,146 Additional reasons for not reporting WPV include fear of retribution or not being believed and not wanting to get involved in litigation.126,143,146 It is essential for HCWs to have access to resources that prepare them to respond to WPV and to ensure workers are empowered to report it.
6. LIMITATIONS
All financial costs in this report are estimates and may not reflect the true cost of workplace and community violence to U.S. hospitals and health systems. Many cost calculations include assumptions as there is limited published literature and data on interested cost components; the study team had to rely on the most recent data available or related data to calculate cost estimates. Assumptions for each cost calculation are included in the corresponding cost component section in this report. It is important to note that all assumptions were made so to be largely conservative in nature, suggesting that the actual financial burden of workplace and community violence to U.S. hospitals and health systems is likely much greater.
7. DISCUSSION
This report estimates the financial and other impacts of violence on hospitals in the U.S. The total financial cost of violence to hospitals is estimated to be $18.27 billion (USD). This estimate includes pre- and post-event cost components. Pre-event costs were estimated to be $3.62 billion (USD) and included costs for trainings, security and staffing, violence prevention programs, policy and procedure development, outreach to build public trust, facility modifications to prevent and mitigate harm, and investments in technology to monitor events. Post-event costs were estimated to be $14.65 billion (USD) and included costs for health care (namely workers’ compensation and unreimbursed costs), staffing, replacement and repair of infrastructure and equipment, and community and public relations costs. The largest contributor to total annual costs came from post-event health care expenses to treat violent injuries.
Beyond the financial burden, there are many other costs of violence to hospitals and health care workers. Health care workers who experience or witness violence can experience many psychological impacts that affect their well-being as well as impact the health system. These psychological impacts lead to reduced workplace satisfaction and productivity, and recruitment and retention challenges, further impacting the burden of violence to hospitals.
Overall, violence is a growing public health problem affecting our communities and health systems. In the current report, we estimated a significantly higher cost of violence to U.S. hospitals compared to a 2016 report which estimated that violence costs $2.7 billion (USD).64 Reasons for the large increase in costs estimated in this report include use of a more expansive definition of violence and components costs than the prior report, and an increase in violent event incidence which impacts post-event costs. Overall, this updated estimate demonstrates the significant burden born by hospitals as a result of violence and costs attributed to treat and prevent violent injuries in the U.S.