Pandemic-Driven Deferred Care Has Led to Increased Patient Acuity in America’s Hospitals
Rise in patient acuity has been a driver of increases in labor, drug, and supply costs for hospitals creating unsustainable financial challenges
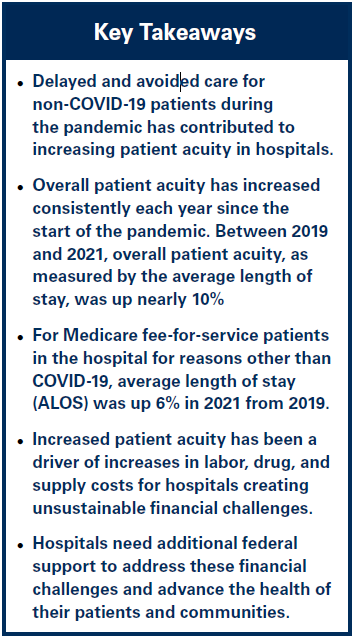 At the outset of the COVID-19 pandemic, communities across America entered mandatory quarantines and temporarily shut down many every day services such as schools, retail stores and libraries. This was done to help control the spread of the virus and protect people and communities. To increase personal and public safety across the country while conserving personal protective equipment (PPE), many hospitals and health systems moved to cancel or delay non-emergency procedures in early 2020. Similarly, many states and the federal government imposed or recommended shutdowns or delays in non-emergency care. At the same time, many Americans avoided or delayed seeking care, including primary care and other specialty care visits.
At the outset of the COVID-19 pandemic, communities across America entered mandatory quarantines and temporarily shut down many every day services such as schools, retail stores and libraries. This was done to help control the spread of the virus and protect people and communities. To increase personal and public safety across the country while conserving personal protective equipment (PPE), many hospitals and health systems moved to cancel or delay non-emergency procedures in early 2020. Similarly, many states and the federal government imposed or recommended shutdowns or delays in non-emergency care. At the same time, many Americans avoided or delayed seeking care, including primary care and other specialty care visits.
COVID-19 treatment is highly complex and resource-intensive, which has been a driver of overall increases in patient acuity during the pandemic. However, non-COVID-19-care has increasingly contributed to rising patient acuity, as well. The confluence of these factors has contributed to patients experiencing more severe disease, in many cases requiring longer hospitalizations and more intensive treatments.
A recent report from Kaufman Hall, with data from Syntellis Performance Solutions, show significant increases in the average length of stay (ALOS) for hospitalized patients during the pandemic compared to pre-pandemic levels. (See Figure #1) Further, data from Strata Decision Technology, a healthcare financial software and analytics firm, show that patients being treated for conditions like cancer and hepatitis, as well as patients undergoing common procedures like appendectomies and mastectomies also experienced significant increases in acuity during the pandemic.1
View the detailed report below.