Encompass Health | U.S.
Post-Acute Care CARE (PAC) | Case Study
Overview
With 168 locations across 38 states and Puerto Rico, Encompass Health is the nation's largest owner and operator of inpatient rehabilitation hospitals (IRF). Encompass Health provides post-acute care for patients who are recovering from life-changing illnesses and injuries, including strokes and other neurological disorders, brain injuries, spinal cord injuries, amputations and complex orthopedic conditions.
Encompass Health is a trusted partner providing individualized, high-quality, compassionate treatment to meet the specific rehabilitation needs and goals of each patient. All Encompass Health hospitals are accredited by The Joint Commission and hold specialty certifications in stroke care, which is a leading cause of long-term disability. In 2024, Encompass Health had over 252,000 patient discharges.
Medicare Advantage: Trends for Inpatient Rehabilitation
Access to IRF care has remained stable for Traditional Fee-For-Service (FFS) Medicare patients, allowing qualified beneficiaries to dependably access intensive post-acute care when referred by their physicians. Today, the healthcare system is changing as more than 54% of older Americans are now covered by private Medicare Advantage (MA) plans. As the number of seniors in MA plans grows, public policy must evolve to ensure patients have appropriate and timely access to the specialized care provided in IRF settings.
MA plans, which differ significantly from Traditional Medicare, are operated by corporate entities and require additional administrative steps before allowing their enrollees to access covered inpatient rehabilitation care, mainly through their use of prior authorization and limited provider networks. Additionally, some MA plans do not partner with any IRFs, meaning patients must pay out of pocket for medically necessary IRF care. In some cases, the most clinically appropriate post-acute care option is financially inaccessible to patients and their families.
Patient Success Story

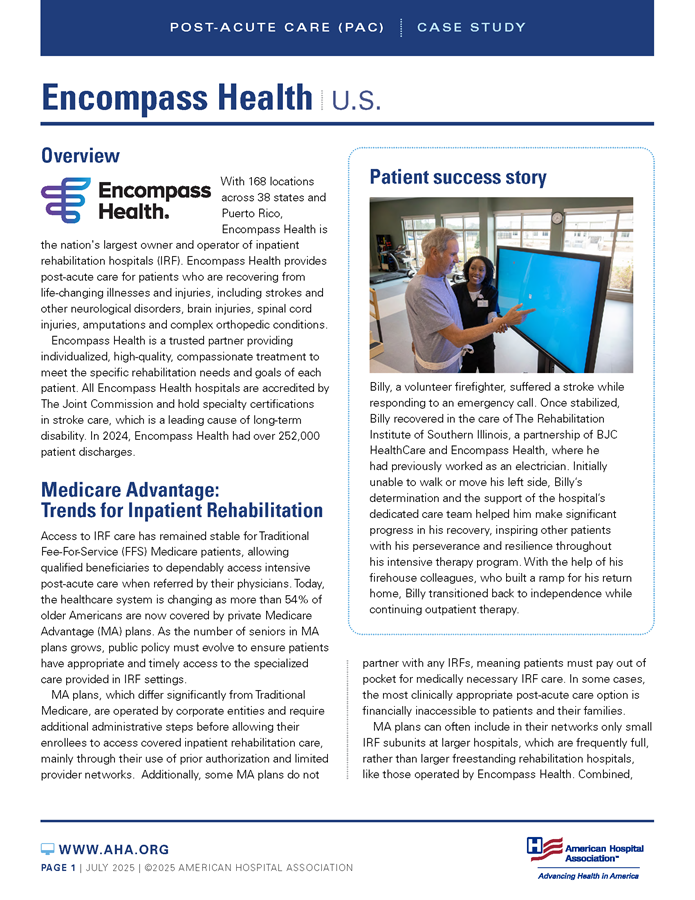
Billy, a volunteer firefighter, suffered a stroke while responding to an emergency call. Once stabilized, Billy recovered in the care of The Rehabilitation Institute of Southern Illinois, a partnership of BJC HealthCare and Encompass Health, where he had previously worked as an electrician. Initially unable to walk or move his left side, Billy’s determination and the support of the hospital’s dedicated care team helped him make significant progress in his recovery, inspiring other patients with his perseverance and resilience throughout his intensive therapy program. With the help of his firehouse colleagues, who built a ramp for his return home, Billy transitioned back to independence while continuing outpatient therapy.
MA plans can often include in their networks only small IRF subunits at larger hospitals, which are frequently full, rather than larger freestanding rehabilitation hospitals, like those operated by Encompass Health. Combined, these challenges have led to a surprising statistic: the utilization rate of IRF care by patients with MA plans is estimated to be about one-third the rate of those in Traditional FFS Medicare.
IRF Care Delivery Challenges
Encompass Health faces a variety of evolving issues that impact care delivery across the country, including:
- Medicare Advantage Prior Authorization: Private Medicare insurer barriers such as prior authorization are often lengthy and taxing on providers’ time and resources and can create dangerous delays in medically necessary and timely patient care.
- Increasingly Complex Patients: The U.S. population is aging, and providers such as Encompass Health are primarily treating patients over age 65 with increasingly complex health care needs. Patients often arrive at Encompass Health hospitals with multiple severe, chronic conditions requiring intensive care. While IRFs are uniquely qualified to treat these complex patients, public policy must ensure patient access to lifechanging IRF care is not restricted.
- Workforce: As with much of the health care industry, finding and retaining well-trained healthcare professionals in the IRF setting continues to be challenging.
The 3-Hour Rule
Patients admitted to an IRF must generally require and reasonably be able to actively participate in three hours of intensive therapy per day, or 15 hours total per week (physical therapy, occupational therapy, speech-language pathology or prosthetics/orthotics therapy). The 3-Hour Rule therapy requirement distinguishes IRF care from other settings and serves as the minimum standard; many patients participate in additional therapy during their stay based on an individualized plan of care.
Solutions to Protect Patient Access to Intensive Post-Acute Care
Medicare Advantage plans are an increasingly popular choice for older Americans, and measures must be taken to ensure that patients who require post-acute care services are able to access them in a timely fashion. Accessing inpatient rehabilitation care as soon as clinically possible is critical for regaining function after a traumatic injury or illness like a stroke. Delays in a patient’s start of rehabilitation risk reducing ultimate recovery potential.
A crucial first step is the addition of inpatient rehabilitation services to the Centers for Medicare & Medicaid Services’s (CMS) network adequacy list requiring all Medicare Advantage plans to include IRFs in their provider networks. This change would ensure that all patients with MA plans are given the option for appropriate post-acute care as prescribed by their physicians on an “in-network” basis.
In addition, CMS should conduct regular audits to ensure that MA providers include robust post-acute care options with sufficient bed spaces and resources to provide the in-network care that patients need.
Finally, policymakers must put safeguards around prior authorization, which can create dangerous delays in patients’ access to care and is often lengthy and taxing on providers’ time and resources that should otherwise be devoted to patient care.