People Matter, Words Matter
Studies have shown that people with psychiatric and/or substance use disorders often feel judged, outside and inside the health care system. This can lead them to avoid, delay or stop seeking treatment. The way we talk about people with a behavioral disorder can change lives – in either a positive or negative manner.
The AHA, together with behavioral health and language experts from member hospitals and partner organizations, will release a series of downloadable posters to help your employees adopt patient-centered, respectful language. Please consider downloading, printing and sharing each poster with your team members and encourage them to use this language both in front of patients and when talking to colleagues. People matter and the words we use to describe them or the disorders they have matter.
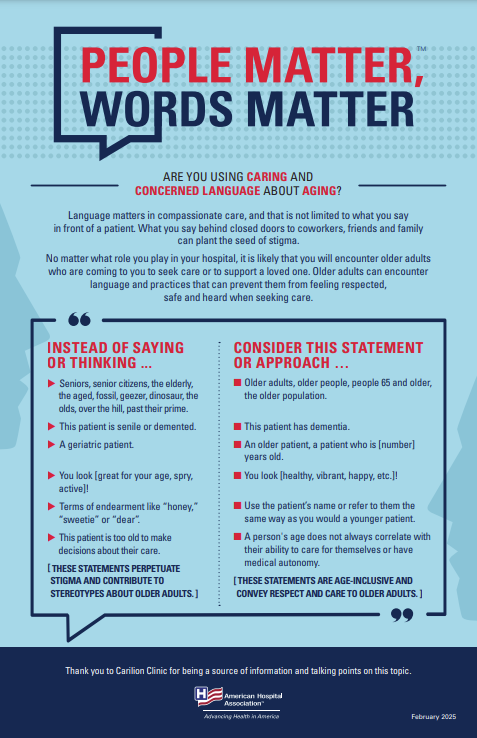
Are You Using Caring and Concerned Language About Aging?
Language matters in compassionate care, and that is not limited to what you say in front of a patient. What you say behind closed doors to coworkers, friends and family can plant the seed of stigma and discrimination. No matter what role you play in your hospital, it is likely that you will encounter older adults who are coming to you to seek care or to support a loved one. Older adults can encounter discriminatory language and practices that can prevent them from feeling respected, safe and heard when seeking care.
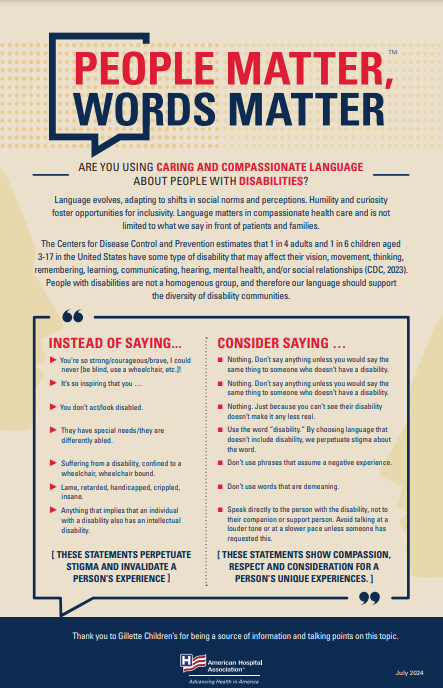
Are You Using Caring and Compassionate Language About People with Disabilities?
The Centers for Disease Control and Prevention estimates that 1 in 4 adults and 1 in 6 children in the United States have some type of disability that may affect their vision, movement, thinking, remembering, learning, communicating, hearing, mental health, and/or social relationships. People with disabilities are not a homogenous group, and therefore our language should support the diversity of disability communities.
Are You Using Caring and Compassionate Language About Eating Disorders?
Language matters in compassionate care, especially in behavioral health care, and is not limited to what we say in front of patients and families. What we say behind closed doors with co-workers can be the seed for stigma and perpetuate discrimination against a person based on a physical or mental health disorder.
According to a 2020 report from the Harvard T.H. Chan School of Public Health, one person dies as the direct result of an eating disorder every 52 minutes. When we talk about eating disorders, we might unintentionally hurt or trigger somebody who is struggling, even when our comments are well-intentioned.
Are You Equipped with the Right Actions and Words to Support Your Colleagues After They Experience an Adverse Event or Distressing Situation?
Health care workers encounter adverse events and stressful situations that may require time and space to process. As health care workers, we all have a role to play in supporting our colleagues who may be struggling with an adverse or stressful situation.
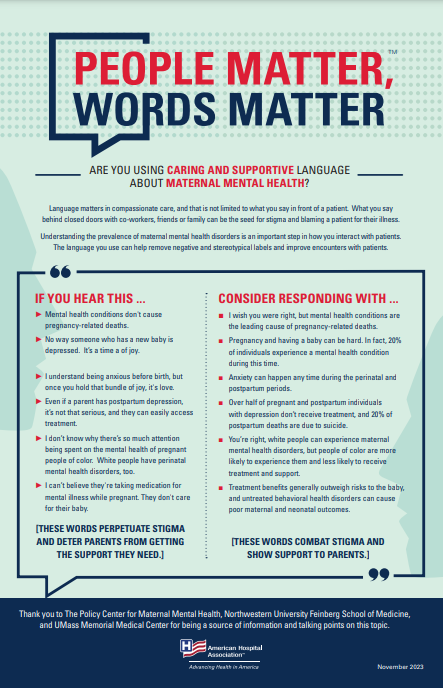
Are You Using Caring and Supportive Language About Maternal Mental Health?
Language matters in compassionate care, and that is not limited to what you say in front of a patient. What you say behind closed doors with co-workers, friends or family can be the seed for stigma and blaming a patient for their illness. Understanding the prevalence of maternal mental health disorders is an important step in how you interact with patients, and the language you choose to use can help remove negative and stereotypical labels and improve encounters with patients and families.
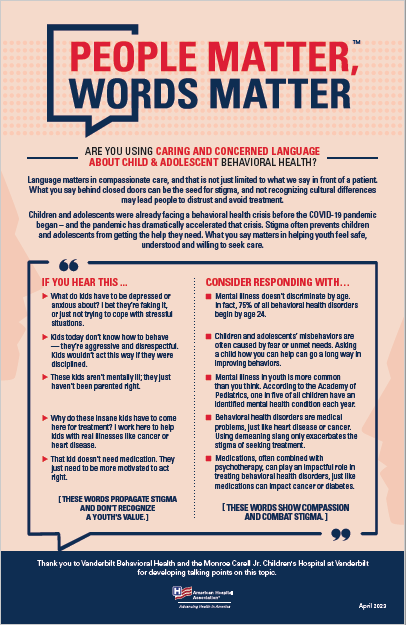
Are You Using Caring and Concerned Language About Child and Adolescent Behavioral Health?
Language matters in compassionate care, and that is not just limited to what you say in front of a patient. What you say behind closed doors to coworkers, friends and family can be the seed for stigma, and may lead people to distrust and avoid treatment.
Children and adolescents were already facing a behavioral health crisis before the COVID-19 pandemic began – and the pandemic has dramatically accelerated that crisis. Stigma often prevents children and adolescents from getting the help they need. What you say matters in helping youth feel safe, understood and willing to seek care.
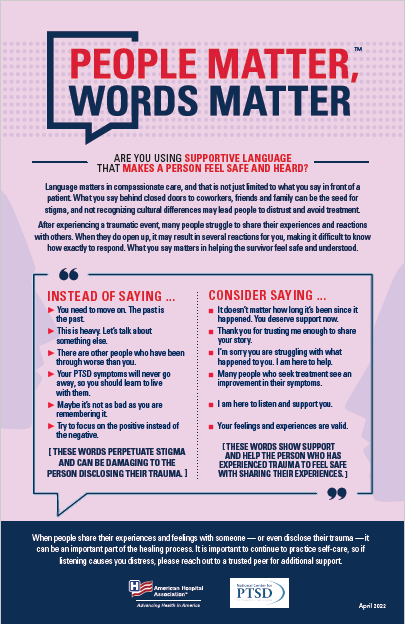
Are You Using Supportive Language that Makes a Person Feel Safe and Heard?
Language matters in compassionate care, and that is not just limited to what you say in front of a patient. What you say behind closed doors to coworkers, friends and family can be the seed for stigma, and may lead people to distrust and avoid treatment.
After experiencing a traumatic event, many people struggle to share their experiences and reactions with others. When they do open up, it may result in several reactions for you, making it difficult to know how exactly to respond. What you say matters in helping the survivor feel safe and understood.
Are You Using Destigmatizing Language About Suicide?
Language matters in compassionate care, especially in behavioral health care, and that doesn’t mean just what you say in front of a patient. What you say behind closed doors with co-workers can be the seed for stigma and perpetuate discrimination against a person based on a physical or mental health disorder. The topic of suicide, and the sometimes-stigmatizing language around it, must be handled with compassion. The language you use can be an important factor in whether or not a person decides to seek care.
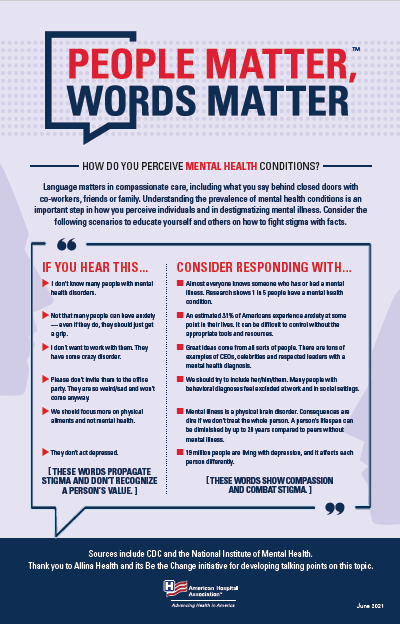
How Do You Perceive Mental Health Conditions?
Language matters in compassionate care, including what you say behind closed doors with co-workers, friends or family. Understanding the prevalence of mental health conditions is an important step in how you perceive individuals and in destigmatizing mental illness. Consider the following scenarios to educate yourself and others on how to fight stigma with facts.
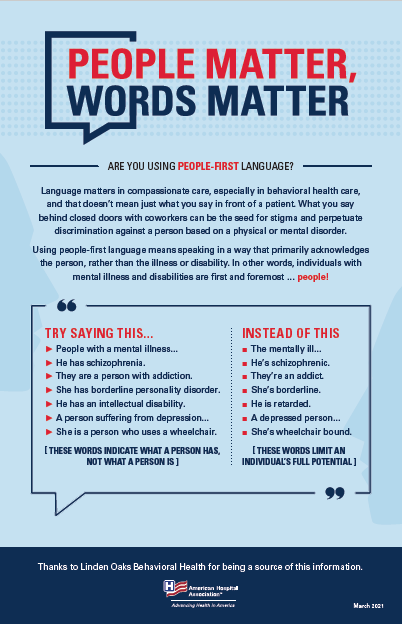
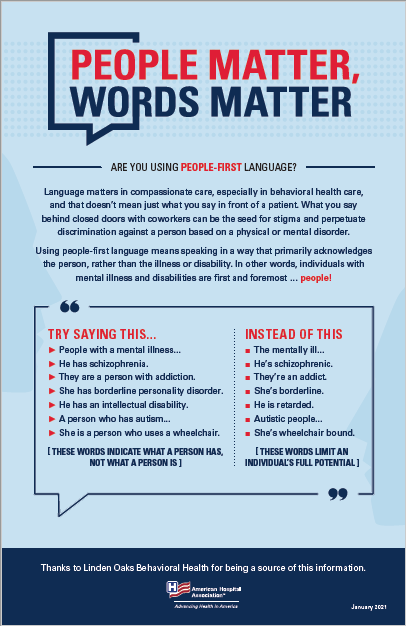
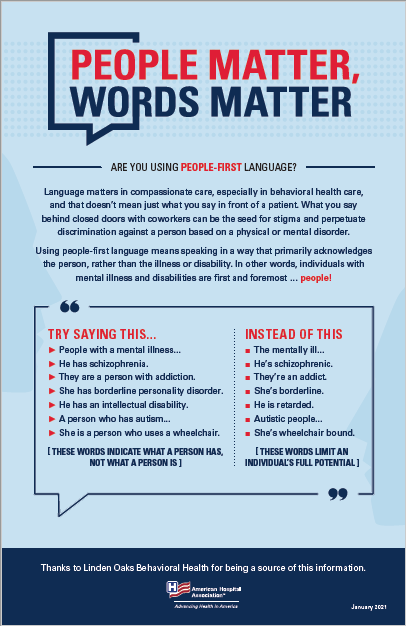
Are You Using People-First Language?
Language matters in compassionate care, especially in behavioral health care, and that doesn’t mean just what you say in front of a patient. What you say behind closed doors with coworkers can be the seed for stigma and perpetuate discrimination against a person based on a physical or mental disorder. Using people-first language means speaking in a way that primarily acknowledges the person, rather than the illness or disability. Thanks to Linden Oaks Behavioral Health for being a source of this poster.
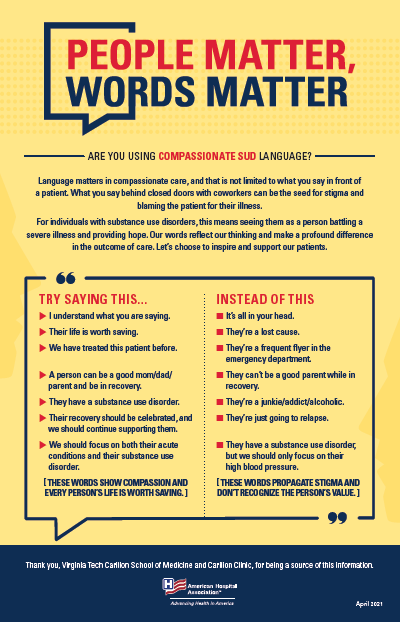
Are You Using Compassionate SUD Language?
Talking to and about an individual with a substance use disorder means seeing them as a person battling a severe illness. Our words reflect our thinking and make a profound difference in the outcome of care. Let’s choose to inspire and support our patients by reducing stigmatizing language. Thanks to Virginia Tech Carilion School of Medicine and Carilion Clinic for being a source of this poster.
Additional Resource(s): Shatterproof: Reversing the Addiction Crisis in the U.S.
Learn More
Chair File: Understanding and Treating Substance Use Disorders by Nancy Agee, AHA Board Chair and President and CEO of Carilion Clinic