

Securing Your Future During Disruption

Health care is on parallel disruption tracks. COVID-19 has provided an unprecedented environment that challenges hospital and health system care delivery, finances, workforce, culture and more. At the same time, provider organizations continue to transform the field in areas like social determinants of health, access to care and emergency response.
 Leaders need to think strategically about the pandemic’s impact on health care in the near and long term and plan for a future defined by resilience and innovation while maintaining an unwavering commitment to high-quality care. Futurescan 2021-2026: Health Care Trends and Implications offers key data and insights on the clinical, operational and strategy landscape, and explores the pandemic’s ramifications.
Leaders need to think strategically about the pandemic’s impact on health care in the near and long term and plan for a future defined by resilience and innovation while maintaining an unwavering commitment to high-quality care. Futurescan 2021-2026: Health Care Trends and Implications offers key data and insights on the clinical, operational and strategy landscape, and explores the pandemic’s ramifications.
Developed by the AHA’s Society for Health Care Strategy & Market Development in conjunction with the American College of Healthcare Executives, the report covers eight critical areas of transformation as seen through the eyes of thought leaders in the field, several of which are summarized here.
Realize the Benefits of Consolidation
The pandemic has vividly illustrated the benefit of consolidation. Organizations with scale have been better positioned to respond to this widespread public health crisis, particularly the critical mass of patients who need intensive care. In preparing for future public health emergencies, Robert C. Garrett, CEO of Hackensack Meridian Health, urges leaders to consider the following:
- Strategic mergers and acquisitions can help organizations increase scalability, expand availability of clinicians, broaden medical expertise and manage the supply chain more effectively.
- Mergers and acquisitions can also broaden an organization’s continuum of care, increasing scalability for large and small organizations alike across geographies.
- Network integration can offer access to specialized clinical expertise and the resources needed to enlarge the enterprise’s scope of services.
 Be More Social in Your Community Focus
Be More Social in Your Community Focus
Bechara Choucair, M.D., senior vice president and chief health officer, leads Kaiser Permanente’s efforts across eight states to help people secure stable housing, healthful food, reliable transportation and social support. He notes that the need for equity in health, human and social services has never been more apparent. Health care organizations are beginning to respond in ways that not only ameliorate social inequities, but also result in positive financial outcomes.
Choucair highlights critical strategies for addressing social inequities that affect overall health, including:
- Target populations. Use data to target the right population and to understand the issues confronting them.
- Partner strategically. Seek local governments, community organizations and businesses already engaged in this work to collaboratively address social factors and inequities that influence health.
- Measure effectiveness. Establishing baselines and measuring the effect of actions on costs and care utilization are key to improvement.
 Value Private Equity in Innovation
Value Private Equity in Innovation
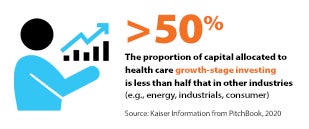
Financial collaborations also will be critical for accessing and adopting competencies that traditionally have not existed in health care, notes Joseph R. Swedish, co-founder and partner at Concord Health Partners and former president and CEO of Anthem Inc. For executives who are considering pursuing private-equity investment to acquire products and services to transform care delivery, he offers these tips.
- Be willing to take on risk. “In the pursuit of innovation, there are pretenders and contenders,” he says. “To be a contender, health care leaders need to be willing to take well-calculated risks.”
- Find the right partner. Due diligence is important in finding a private-equity expert in the field in which an organization wants to innovate. Sector specialization is critical in health care given its complexities and the changing regulatory environment, Swedish says.
- Balance strategies. A private-equity partnership could have a 5- to 10-year timeline. Look for a partner that shares your organization’s values and aligns with strategic goals.
To learn more, download the Futurescan 2021-26 report.



