Survey Brief: Drug Companies Reduce Patients’ Access to Care by Limiting 340B Community Pharmacies
November 2022
Background
In 1992, Congress created the 340B Drug Pricing Program to allow providers that treat high numbers of uninsured and low-income patients the ability to purchase certain outpatient drugs at discounted prices and use those savings to “stretch scarce federal resources as far as possible, reaching more eligible patients and providing more comprehensive services.” For 30 years, the program has been a critical lifeline for many eligible providers and their patients, especially in the face of chronic underpayments from Medicare and Medicaid.
However, within the last several years, the program has come under a new threat by Big Pharma that only serves to benefit their bottomlines at the expense of patients and providers. In July 2020, in violation of federal law, six drug companies announced their decision to end discounted pricing to 340B hospitals for arrangements established with community and specialty pharmacies. These federally authorized arrangements between 340B hospitals and community and specialty pharmacies are a critical component of the 340B program that allows providers to expand access to many drugs — including those used to treat rare and complex conditions such as some cancers — for the patients and communities they serve. In particular, these arrangements improve access by allowing both hospitals and pharmacies to coordinate care and ensure that drugs needed by the patients cared for by 340B hospitals are available to them at their local pharmacy.
In response to the unlawful actions by drug companies for failing to provide discounts through community pharmacies, the Health Resources and Services Administration (HRSA), which oversees the 340B program, exercised its authority to refer these companies to the Office of Inspector General (OIG) to impose civil monetary penalties. Several drug companies then filed lawsuits challenging the government’s authority to enforce penalties against them citing that the law did not require them to offer discounts through these authorized arrangements with community pharmacies. In the face of these ongoing legal proceedings, more drug companies have ended their discounted pricing to providers. As of October 2022, 18 drug companies have adopted these restrictive policies to the severe detriment of 340B hospitals and their patients. The AHA has supported HRSA in its efforts to enforce the requirements for drug companies set forth in the 340B statute.
Survey Results
 In April 2022, the American Hospital Association (AHA) conducted a brief survey of more than 300 hospitals and health systems to understand the financial and operational impact of drug companies’ actions to limit 340B pricing to 340B hospitals with community and specialty pharmacies.
In April 2022, the American Hospital Association (AHA) conducted a brief survey of more than 300 hospitals and health systems to understand the financial and operational impact of drug companies’ actions to limit 340B pricing to 340B hospitals with community and specialty pharmacies.
The survey results show:
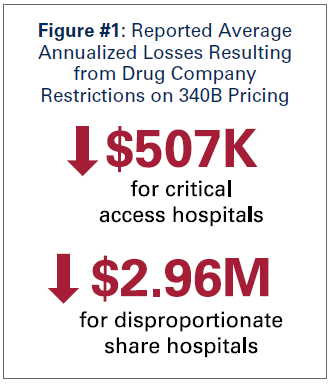
- The average 340B critical access hospital (CAH) - hospitals with 25 beds or less serving rural communities - reported losses of approximately $507,000, while the average 340B disproportionate share hospital reported losses of $2.96 million (see figure 1). CAHs represented 45% of survey respondents and DSH 43% of survey respondents.
- On average, CAHs reported 44% of their total 340B savings coming from community and specialty pharmacies, with
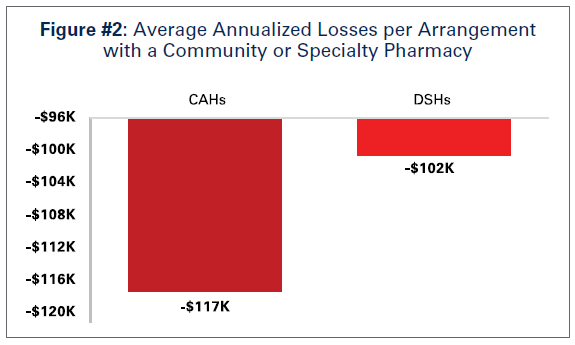 several CAHs reporting that their entire 340B savings come from these arrangements. 340B CAHs had a slightly larger financial impact than 340B DSH hospitals when looking at a per arrangement basis (see figure 2).
several CAHs reporting that their entire 340B savings come from these arrangements. 340B CAHs had a slightly larger financial impact than 340B DSH hospitals when looking at a per arrangement basis (see figure 2). - Overall, 10% of responding hospitals reported $10 million or more in financial impact, illustrating the magnitude of the harm that drug companies’ actions have on 340B hospitals and their ability to care for their patients.
- The survey results also revealed that, on average, approximately 20% of arrangements with a community or specialty pharmacy had no drug purchase volume. These “no volume on the books” pharmacy arrangements are primarily an outcome of large pharmacy chain policies requiring covered entities to enter into arrangements with all pharmacies in a given area. As a result, the actual number of “active” arrangements with community and specialty pharmacies are much lower than what hospitals are required to report to HRSA. This finding demonstrates how drug companies inaccurately portray growth in the program.
Discussion
The survey results make it clear that drug companies’ actions to limit 340B pricing through community and specialty pharmacies are harming 340B hospitals and their patients. In fact, the financial impacts reported by hospitals in this survey likely understate the full impact. That is because, when this survey was fielded in April 2022, 14 drug companies had imposed limits on 340B pricing; that number has now grown to 18 drug companies affecting hundreds of drugs.
While drug companies claim that their efforts to limit 340B pricing through community pharmacies are intended to mitigate supposed abuse of the program, they fail to acknowledge the critical purpose these pharmacies serve in the delivery of care to patients or how the only benefit of their actions accrues to them in the form of smaller discounts they must provide. At a minimum, these pharmacy arrangments allow a 340B hospital to provide broadened access to drugs in patients’ own communities. As such, these arrangements allow both the hospital and the pharmacy to coordinate both the inventory of drugs (to ensure patients who need a particular drug have access to that drug at their local pharmacy) and the provision of care (to ensure that patients are receiving the drugs they were prescribed as part of their treatment).
Benefits to Patients Served by Small and Rural Health Care Providers
For smaller hospitals and those serving primarily rural communities, many of which do not operate their own in-house pharmacy, the only avenue for their patients to access drugs covered under the 340B program is to purchase them through a community or specialty pharmacy. Having an arrangement with that community or specialty pharmacy allows many rural hospitals the only opportunity to earn savings from the 340B program and use those savings to furnish critical programs and services for their rural patients. As a result, rural patients, many of whom are unable to travel long distances for care, are not only able to get access to drugs at their local pharmacies, but also get access to a whole range of services supported directly by 340B program savings such as behavioral health and chemotherapy in their local communities.
Benefits to Patients Served by DSH Hospitals
On the other hand, a larger hospital that serves a more diverse and expansive area and may operate one or more in-house pharmacy may decide to enter into an arrangement with a community or specialty pharmacy because their patients come from a large area and may not be able to travel to the hospital’s in-house pharmacy to receive their drugs.
Many larger 340B hospitals, which tend to be DSH hospitals, also are large academic medical centers that care for the sickest and most complex patients. As a result, they serve as centers of excellence for specific diseases and attract patients from across the country. In particular, many of these 340B DSH hospitals are certified by the Joint Commission as Advanced Comprehensive Stroke Centers, meaning these hospitals care for some of the most complex stroke cases across the country. Similarly, many 340B DSH hospitals also serve as NCI-designated comprehensive cancer centers where they treat the sickest and most complex cancer patients, and provide their patients access to cutting-edge treatments and clinical trials. As a result, these 340B DSH hospitals must be able to establish arrangements with pharmacies outside of their immediate geographic area, so that patients who travel long distances to the hospital for specialized care can still access needed drugs at their local pharmacies back home.
Further, because DSH hospitals see the most complex patients, they also utilize some of the highest-cost, specialty drugs that are often in limited distribution. Patients can only access these drugs through certain specialty pharmacies, and as a result, 340B hospitals must establish arrangements with these pharmacies to ensure patients receive the drugs they need, when they need it..
A Critical Lifeline Throughout the COVID-19 Pandemic
Perhaps the most compelling argument in support of 340B hospitals working with community and specialty pharmacies can be seen throughout the COVID-19 pandemic. Patients across the country often were unable to and/or fearful of receiving care at the hospital. In fact, according to a 2020 survey conducted by the Centers for Disease Control and Prevention (CDC), 4 in 10 adults reported delaying their care due to concerns related to the pandemic. As a result, many of these patients relied on receiving drug treatments at their local community pharmacies or through mail-order specialty pharmacies.
These established pharmacy relationships allowed hospitals to ensure that their patients were able to receive the drugs they were prescribed, even if those patients couldn’t access those drugs at the hospital. Additionally, 340B hospitals were able to use these arrangements to ensure their patients had access to drugs where there were shortages due to supply chain constraints wrought by the pandemic. Without these arrangements in place, patients of these 340B hospitals may have been unable to access those drugs, potentially jeopardizing their health and well-being.
Just as the pandemic has reinforced the need for 340B hospitals to maintain arrangements with community and specialty pharmacies for the benefit of their patients, drug companies have undermined the programs’ benefits by denying 340B pricing and reducing savings to 340B hospitals. The data show that the financial impact is immense whether a 340B hospital is small or large, urban or rural. These impacts are especially problematic given the many financial pressures hospitals currently face, from historic increases in inflation to mounting labor and non-labor costs.Though these cost pressures are not unique to 340B hospitals, the additional financial impact from the denial of 340B pricing through authorized arrangements with community and specialty pharmacies have certainly exacerbated the challenges for these hospitals. Collectively, 340B hospitals report that these financial pressures have put critical patient programs and services at risk as well as their ability to offset increased costs in other areas like labor and drugs. While the specific impacts of drug companies’ policies to limit 340B pricing vary among 340B hospitals, several themes of impact are consistent across the board:
- Unable to hire adequate staff (e.g., nurses and respiratory therapists) to mitigate critical staffing shortages and necessary to care for patients
- Reduced community outreach activities including things like offering free COVID-19 testing and vaccinations
- Reduced the scope of certain programs that are targeted for a hospital’s underserved patients such as mobile treatment clinics in rural areas
- Limited or temporarily closed down certain specialty clinics and service lines that are critical like OBGYN and oncology
Given these impacts, denying 340B pricing to 340B hospitals is an unsustainable reality for these hospitals. The results of this survey add to the growing body of literature illustrating the harmful impacts that drug companies’ actions are having on 340B patients and providers. In fact, the only beneficiaries of drug companies’ actions to limit 340B pricing through authorized arrangements with community and specialty pharmacies are the drug companies themselves, and the financial windfall they receive as a result of limiting the 340B program comes at the expense of patient care. Therefore, it is in the interest of patients, providers and policymakers to ensure that drug companies immediately cease their unlawful efforts to dismantle a program that has been successful for over 30 years in providing access to care for millions of Americans.