

Virtual Care’s Post-COVID-19 Future Comes into Focus

The COVID-19 pandemic forced Americans to rapidly and without warning pivot to telehealth at levels exponentially higher than before the pandemic. So, what’s next?
With the White House’s recent executive order on improving rural health and telehealth access, the future of virtual care is becoming clearer. The order includes directives to: launch a new payment model for rural health care; develop and implement a strategy to improve rural health care infrastructure; create a report describing policy initiatives to improve rural health; and propose a regulation that would extend certain telehealth flexibilities.
The order also directs the HHS secretary to review within 60 days the following temporary measures put in place during the COVID-19 public health emergency and to extend these measures as appropriate beyond the pandemic:
- The additional telehealth services offered to Medicare beneficiaries.
- The services, reporting, staffing and supervision flexibilities offered to Medicare providers in rural areas.
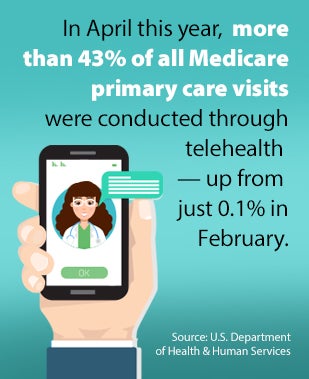
These measures should help support continued growth in the delivery of primary care telehealth services, which have ballooned during the pandemic. More than 43% of all Medicare primary care visits were being conducted through telehealth in April, according to a recent Department of Health & Human Services report. That's up from just 0.1% in February.
 And it’s not just hospitals and health systems that are experiencing this growth. Virtual care service disruptors and payers also are greatly expanding their reach in the telehealth market.
And it’s not just hospitals and health systems that are experiencing this growth. Virtual care service disruptors and payers also are greatly expanding their reach in the telehealth market.
Teladoc and AmericanWell saw huge spikes in demand for their primary care virtual services. Teladoc conducted more than 2.8 million virtual visits in the second quarter, more than triple the same period last year, while its U.S. membership nearly doubled year over year to 51.5 million. And its recently announced merger plans with the diabetes and hypertension digital coaching company Livongo will satisfy Teladoc’s long-held desire to expand into chronic disease management.
American Well, meanwhile, in late May told CNBC that on average it has seen a 1,000% increase in telehealth visits during the pandemic in some regions and as much as 4,000% in others.
That kind of growth is leading venture capitalists to provide more money to companies like American Well, which raised another $194 million in May to help it keep up with skyrocketing demand.
Startup payer Oscar recently said it will greatly expand its national presence in virtual health care services due in large part to what has occurred during the pandemic. The company, which competes with behemoths like UnitedHealthcare and Anthem, will expand into four new states (Oklahoma, Iowa, North Carolina and Arkansas), while also adding new counties in Arizona, California, Florida, Pennsylvania and Ohio. Oscar will also sell a low-cost virtual primary care option to many of its customers in response to COVID-19; the plan will include unlimited no-cost virtual visits with a primary care physician and urgent care.
With all these rapid changes taking place, health care providers will need to advance their virtual care strategies quickly and provide the infrastructure and rapid response that consumers have come to expect during the pandemic. Here are some important issues to keep in mind:
- Continue to provide telehealth services as an option to protect patients and staff from COVID-19.
- Expand virtual interactions for both primary and specialty care to maintain continuity of care and avoid negative consequences of delayed care.
- Partner with rural and general acute care hospitals to create new access to specialty and subspecialty services.
- Offer specialty consults directly to consumers who are hesitant to travel during the pandemic.
- Use tele-ICU to monitor patients to enhance outcomes, maximize use of staff and reduce the use of personal protective equipment.



