

Specialist and Private Practices Take Severe Blow During Pandemic

COVID-19’s impact on health care has been deep and broad and new research shows physicians are being especially hard hit, which could have significant implications for provider organizations and patients.
Published last month, the first of a three-part survey report from The Physicians Foundation paints a sobering picture of the existential threat the pandemic has posed to many physician practices.
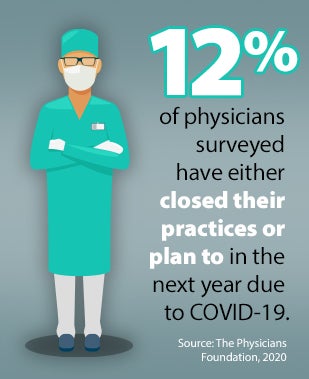
Survey data revealed that 8% of respondents have closed their practices, with more than three-quarters of this group being specialists. That could equate to as many as 16,000 practices nationally based on SK&A market research data. Another 4% said they plan to close their practices within 12 months as a result of COVID-19.
 More than three-fourths of the physicians who closed their practices were in private practice or partners. The report also notes that the pandemic has imposed severe economic strain on many private practices that often lack the financial resources of hospital systems, academic medical centers and large, multifacility medical groups.
More than three-fourths of the physicians who closed their practices were in private practice or partners. The report also notes that the pandemic has imposed severe economic strain on many private practices that often lack the financial resources of hospital systems, academic medical centers and large, multifacility medical groups.
The pandemic also has taken a toll on physicians’ income. Nearly three out of four respondents (72%) said their income has dropped during the pandemic, with more than half of this group seeing a decline of 26% or more; nearly one-fourth experienced at least a 51% income drop over the four months before the survey was conducted (between July 15 and 26).
Much of the decline in specialists’ income can be traced to postponement of nonemergent procedures and a general reluctance among patients to seek specialty care during the pandemic. Income reductions of this level likely will prove unsustainable and could lead to further practice closures or physician retirements, the report states.
Even as primary care doctors, specialists and provider organizations now work to reduce the backlog of needed nonemergency procedures, respondents say there will be lasting health consequences on their communities. Nearly three-quarters of the more than 3,500 respondents believe there will be a rise in more serious health conditions because patients are delaying the care they need during the pandemic.
The survey findings underscore several important points for health care leaders:
- Maintain close relationships with physicians, whether they are employed by provider organizations or are in private practice. This is essential during times of crisis and with potential doctor shortages looming. Both parties must be able to count on each other. And to build the care delivery models that will be needed going forward, clinical and administrative teams must work together.
- Continue to question assumptions about traditional ways of doing things. Many facilities did away with waiting rooms as the pandemic unfolded and reexamined triage and other processes. Explore what lessons your organization has learned during the pandemic and what changes are still needed or should become permanent.
- Develop a firm understanding of the behavioral and mental health needs of your team and community. Whether your organization is seeing a large or small number of COVID-19 patients during this crisis, everyone is undergoing a traumatic experience. Your team’s world has changed radically in a short period. Be aware of what impact that may have on your organization in the future.
To learn more about how to leverage your learning and experiences during COVID-19 and the role of collaboration between clinical and administrative leaders, listen to two recent AHA Physician Alliance podcasts: One discussion features Bruce Flanz, president and CEO, and Antonietta Morisco, M.D., anesthesiologist and chair of anesthesia, both at Medisys Health Network, and the other includes leaders from Henry Ford Health System.



