

Studies Find That Remote Monitoring Advanced Care During Pandemic

Remote patient monitoring (RPM) has been a key component of value-based strategies like hospital-at-home and in certain specialties like palliative care, as well as managing patients with chronic diseases. During the pandemic, many provider organizations rapidly scaled their RPM programs to assess patients of varying acuities.
Only recently, however, have large-scale studies surfaced that measure the impact of RPM programs during the current health crisis. The findings from this research could help hospitals and health systems going forward as they continue efforts to reduce costs and improve outcomes.
Several recent studies documented how RPM prevented avoidable hospital readmissions and improved patients’ recovery from the virus.
A recent Mayo Clinic study, for example, documented how its RPM program prevented avoidable hospital readmissions and improved patients’ recovery from the virus. The analysis of data from more than 7,000 patients across 41 states reported that its two-tiered RPM program with nursing support was safe, effective and led to positive outcomes, including:
- High patient-engagement levels.
- Low hospitalization rates.
- Low 30-day mortality rates.
The health system rapidly scaled and modified its existing RPM program that was developed to treat patients with such complex, chronic conditions as congestive heart failure and chronic obstructive pulmonary disease to meet the needs of COVID-19 patients.
A Targeted RPM Approach
Two separate COVID-19 RPM care models with differing technological capabilities and monitoring intensities were utilized to support patients at low and high risk for severe illness. The technology-enabled monitoring comprised twice-daily, patient-reported symptom assessments and vital signs obtained from peripheral medical devices, including pulse oximeters, thermometers and blood-pressure monitors.
Centralized RPM-registered nurses responded to the technology-generated alerts and utilized standardized care pathways for clinical assessments and patient management, including escalation to the COVID-19 care team physicians.
The results were impressive.
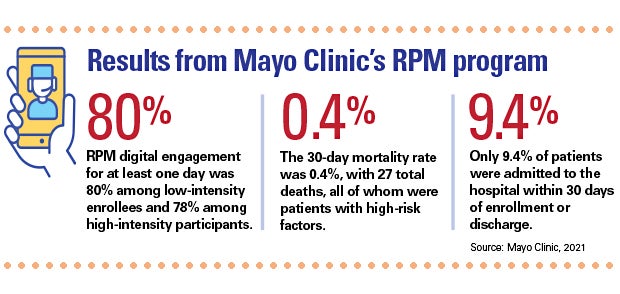
- RPM digital engagement for at least one day was 80% among low-intensity enrollees and 78% among high-intensity participants.
- Compliance with care plan tasks was 61.6% among low-intensity patients and 72.5% among high-intensity patients.
- Only 9.4% of patients were admitted to the hospital within 30 days of enrollment or discharge.
- The 30-day mortality rate was 0.4%, with 27 total deaths, all of whom were patients with high-risk factors.
The study results support the Centers for Medicare & Medicaid’s 2021 expansion of reimbursement for qualifying remote patient monitoring program services for acute-condition management.
Evidence Mounts on RPM’s Value
A similar Kaiser Permanente study published in July found that deploying RPM to treat COVID-19 patients proved effective in preventing readmissions and improving recovery from the virus.
The study found that only about 10% of the 13,055 patients were admitted to the hospital based on their reported symptoms. Only 0.2% of patients died while participating in the remote monitoring program. These patients were usually 60 or older and more likely to have had existing comorbidities like obesity or hypertension. And 95.5% of patients recovered from COVID-19, completing the RPM program in an average of nine days.
The study also found high satisfaction among participants. More than 94% of the responding patients said they were satisfied with the quality of care and would recommend the program to others.
Elsewhere, a study conducted by the Department of Veterans Affairs’ Office of Connected Care credited its high success rate in treating veterans at home during the pandemic largely due to its nearly two decades of experience with RPM.
The study notes that the VA saw surges in veterans diagnosed with COVID-19 in April and July 2020, and during the winter of 2020-21, when the agency twice surpassed 2,000 daily admissions into the program. Throughout those surges, the VA maintained and increased its satisfaction rate for the program, which regularly stands at about 90%.
For more on the value of digital solutions to allow care teams to use more standardized protocols, listen to the AHA’s Seven in Seven podcast series. The reports feature seven-minute conversations with seven experts who highlight ways technology-enabled services improve perinatal care.



