Data Brief: Health Care Workforce Challenges Threaten Hospitals’ Ability to Care for Patients
More than 20 months after the first cases of COVID-19 were reported in the U.S., the pandemic continues to affect communities across the country and has pushed our health care system to the brink, with the latest surge from the delta variant raising new challenges.
To date, there have been more than 45 million cases of COVID-19 in the U.S. and nearly three-quarters of a million deaths. Throughout the pandemic, hospitals and health systems and their workforces have remained on the front lines mobilizing resources to ensure access to care for the patients and communities they serve. In the face of mounting financial challenges, estimated to be $54 billion in net income losses in 2021 alone, hospitals have cared for over 3.2 million COVID-19 patients since August of last year.
 In addition to these billions of dollars in losses for hospitals, hospital and health care workers have been on the front lines battling COVID-19 for nearly two years, and the pandemic has placed a significant toll on them.
In addition to these billions of dollars in losses for hospitals, hospital and health care workers have been on the front lines battling COVID-19 for nearly two years, and the pandemic has placed a significant toll on them.
A Kaiser Family Foundation/ Washington Post poll found that about 3 in 10 health care workers considered leaving their profession, and about 6 in 10 said pandemic-related stress had harmed their mental health. In addition, a survey by AHA’s American Organization for Nursing Leadership found that one of the top challenges and reasons for health care staffing shortages reported by nurses was “emotional health and wellbeing of staff.” This level of burnout coupled with ongoing COVID-19 surges, as well as other existing health care workforce pressures, has left hospitals across the country to contend with critical staffing shortages.
A sufficient, healthy workforce is foundational to maintaining access to high quality care, especially as hospitals are strained by crises such as surges in COVID-19 hospitalizations. Consequently, staffing shortages have driven an increase in wages forcing hospitals to invest significant resources to recruit and retain staff. In the face of an ongoing pandemic, such investments in labor have only exacerbated hospitals’ existing financial hardships, with over one-third of hospitals projected to be in the red by year’s end and a median operating margin that’s 10% to 11% below pre-pandemic levels.
Despite increasing demand for health care services, hospital employment data indicates a critical shortage of staff necessary to meet that demand.
- A number of factors led to hospital employment experiencing steep declines after the U.S. government declared COVID-19 a public health emergency in March 2020. While hospitals have worked to ramp up staffing, they still have not regained all of the staff they would need. Since February 2020, hospital employment has decreased by nearly 94,000, including a decrease of over 8,000 between August 2021 and September 2021 alone.
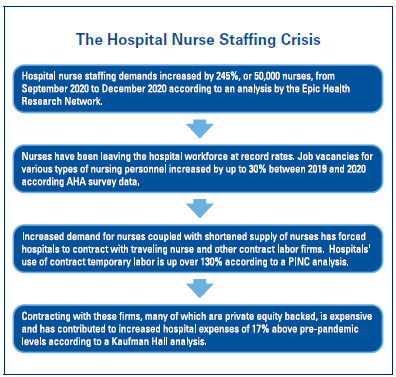
- Job vacancies for various types of nursing personnel increased by up to 30% between 2019 and 2020, according to an analysis of AHA survey data. There also was a 31% increase in job vacancies for respiratory therapists, who often are part of the critical care team for COVID-19 patients, between 2019 and 2020.
- Staff turnover due to COVID-19 pressures has increased from 18% to 30% for some hospital departments (e.g., emergency, intensive care units, and nursing).
- These pressures are expected to persist. An analysis of EMSI data found that there will be a critical shortage of 3.2 million health care workers by 2026 illustrating the magnitude of the problem facing the health care field, namely hospitals and health systems.
The critical staffing shortage of health care workers has forced hospitals to incur increased costs during the ongoing pandemic.
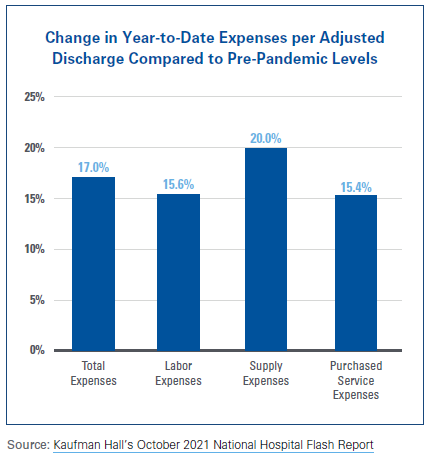
- Hospitals have experienced a 15.6% increase in labor expenses per adjusted discharge compared to September 2019. Hospitals also have experienced increases in most other categories of expenses, including purchased service expenses, which contain costs associated with acquiring contract labor. Together, the increases in labor expenses and other expense categories indicate the magnitude of the impact that health care labor supply issues have had on hospital finances.
- The number of full-time equivalent (FTE) staff per adjusted occupied bed has gone down nearly 3% from pre-pandemic levels. This has occurred while patient acuity (as measured by patient length-of-stay) has increased by nearly 6% since pre-pandemic levels. These two trends mean fewer staff available to treat sicker patients.
- An analysis of workforce data found that staffing shortages have cost hospitals $24 billion over the course of the pandemic, with an additional $3 billion in acquiring personal protective equipment (PPE) for staff.
- Credit rating agency Moody’s has forecasted a decrease in hospital margins over the next year due to a combination of wage inflation, the use of expensive contract nurse staffing firms, and the expansion of hospital worker benefits in order to retain employees.
- According to credit rating agency Fitch Ratings, labor expenses (salaries and benefits) are the largest expense category for hospitals, making up more than 50% of a hospital’s total expenses. Between February 2020 and August 2021, average hourly wages for hospital employees have risen 8.5%, and is unlikely to subside anytime soon.
As the nation continues to grapple with the COVID-19 pandemic, hospitals and health systems nationwide have stepped up in many ways to serve the needs of their communities. Though hospital volumes have seen a sluggish recovery to pre-pandemic levels, there has been growing demand for services with an associated rise in patient acuity. Yet, this increased demand has not been met with an increased supply of staff, creating a staffing shortage that has forced hospitals to incur significant costs to recruit and retain employees.
While government support to date has been critical in helping hospitals weather the early financial challenges they have faced, the current staffing shortage presents a whole new set of challenges that will undoubtedly strain an already precarious financial situation. The AHA continues to urge Congress to prioritize funding and policies to expand and retain America’s health care workforce so that patients and communities can continue to access care.