Strengthening the
Health Care Workforce
Strategies for Now, Near and Far
Section 1 | Supporting the Team
Supporting Behavioral Health
Health care workers suffered emotional and physical strain from treating COVID-19 patients; not only did they risk exposure, but the crisis also hurt their mental health, contributing to anxiety, stress, depression and loneliness.
A recent study found that 93% of health care workers reported stress, 86% reported anxiety, 77% reported frustration, 76% reported exhaustion and burnout, and 75% said they were overwhelmed. Yet just 13% of front-line health care workers say they received behavioral health services.
As illustrated below, responses follow an up and down trajectory, however, the COVID-19 pandemic has stretched this response due to ongoing surges and little time to complete reconstruction. 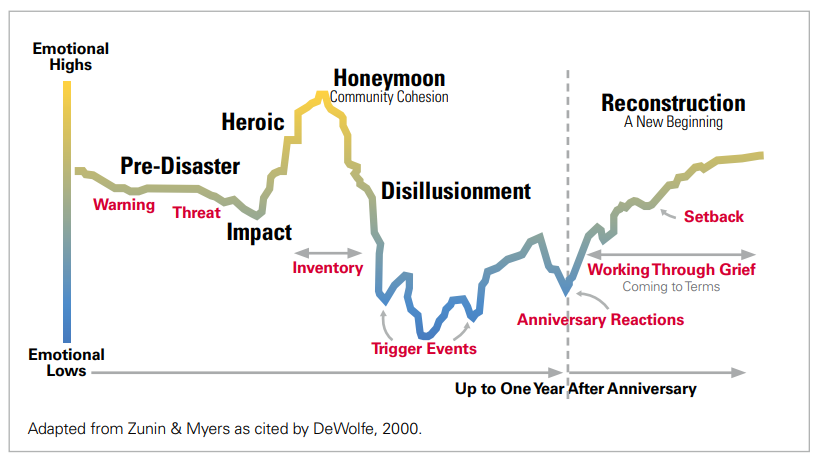
Reducing stigma and improving access to behavioral health services for the health care workforce, combined with fostering human resilience can improve mental and often physical health, reduce the total cost of care, reduce suicide, and support a healthy workforce.
Top Takeaways for CEOs
1 Identify and promote ways your team can access the full continuum of behavioral health services.
2 Remove stigma about behavioral health treatment.
3 Build and sustain a culture of psychological safety. Consider providing training in mental health awareness or first aid.
-
It is important to understand the difference between burnout and behavioral health disorders. Burnout is a long-term stress reaction defined by having at least one of the following symptoms: 1) emotional exhaustion; 2) depersonalization, including cynicism and a lack of empathy; and 3) a low sense of personal accomplishment. Burnout can be a contributing factor or trigger for mental illness, but individuals can be burned out without having a psychiatric or substance use disorder.
Stress responses land on a spectrum based on preparedness and individual resilience. For more resources related to addressing health care worker burnout, see Chapter 1.
-
Building on the inventory of well-being efforts from the previous chapter, identify how your organization’s clinical and non-clinical teams (and their families) can access behavioral health treatment.
- The inventory should review access to the full range of the behavioral health service continuum. The inventory also should include access to integrated physical and behavioral health services, as 70% of adults with a behavioral health disorder also have a physical health condition, and costs are 75% higher. The continuum also should be able to meet the unique needs of children, adolescents, adults and geriatric patients.
-
Next, inventory the adequacy of your existing network of behavioral health providers. Key questions include:
- Are there sufficient clinicians who take the insurance coverage of your employees?
- Are providers taking new patients?
- Are providers physically accessible?
- What are the providers or staff linguistic capabilities?
- Is there access to subspecialty care as noted above: child & adolescent, geriatric?
- What is the wait time to access a therapist for your health plan, employee assistance program (EAP)?
- Are there options for hospital staff to see a behavioral health provider not affiliated with your organization and remain covered by your health plan?
- Is there access to behavioral health via telehealth or other digital treatment platforms?
-
For organizations that do not have behavioral health services or would like to supplement the services offered, consider adding these questions:
- What community-based behavioral health resources exist?
- Is there a Community Mental Health Center, Certified Community Behavioral Health Center, and/or a Federally Qualified Health Center with integrated behavioral health services?
- Are these services accessible to your team members?
-
STANDARDS
CMS Finalizes CY 2024 Medicare Advantage Rule
Network Adequacy Standards and Enforcement | KFF
Network Adequacy - NAIC -
DIRECTORIES
Locate Community Mental Health Centers (list includes only members of the National Council on Mental Wellbeing)
Certified Community Behavioral Health Clinic Locator
Federally Qualified Health Centers and Look-Alikes
- Verify that the health plan(s) offered to your employees are compliant with the Mental Health and Addiction Act Parity Act of 2008
-
Determine the level of staff awareness regarding existing behavioral health resources and identify a plan to bolster communication outreach as needed.
- Consider surveying staff to obtain a baseline awareness level of EAP services, health plan coverage, the range of behavioral health clinicians and services available to them.
- Identify existing data for your team’s use of existing behavioral health resources. If not, consider working with your EAP, health plans and others to establish a baseline use of resources. Review use over time to direct future needs.
- Consider whether stigma presents a barrier to your team accessing services. Communications to bolster psychological safety and clear messaging on confidentiality, job security and licensure may be needed.
-
Identify if your organizational culture consistently supports health-seeking behaviors for mental health/ substance use disorders.
-
Examine policies to determine if they support mental wellbeing. For instance:
- Does your sick leave policy address behavioral health disorders?
- What is your hospital’s policy on leave for family matters?
- Do you provide any digital solutions to support meditation, self-reflection or whole health?
- Do you encourage staff to have a primary care physician and/or incentivize annual physicals, including screening for behavioral health?
-
Examine policies to determine if they support mental wellbeing. For instance:
-
The assessment also should include questions that are uniquely related to physicians and advanced practice providers:
-
Do your organization’s credentialing questions perpetuate stigma of behavioral health disorders?
- Consider adopting questions that focus on current impairment, encourage treatment, and do not distinguish between psychological and physical conditions and are recommended by the Federation of State Medical Boards.
-
POLICY
Remove Intrusive Mental Health Questions from Licensure and Credentialing Applications
Federation of State Medical Boards
-
Are your affiliated clinicians aware of your state’s Physician Health Program (PHP)? PHPs are a confidential resource for physicians, other licensed health care professionals, or those in training suffering from addictive, psychiatric, medical, behavioral or other potentially impairing conditions.
-
DIRECTORIES
State PHP Directory
-
DIRECTORIES
-
Do your organization’s credentialing questions perpetuate stigma of behavioral health disorders?
-
Create a culture of psychological safety where all staff feel safe to speak out and seek out treatment to improve their mental health or address substance use disorders. This requires a cultural shift that should involve all stakeholders.
-
TOOLS
Reduce Stigma: People Matter Words Matter is AHA’s stigma reduction campaign to help overcome actions that cause people to avoid, delay or stop seeking treatment. How we talk about behavioral disorders can change lives, positively or negatively.
Nine ways to fight mental health stigma recommends actions by the National Alliance on Mental Illness. -
Tell your own story: Many have remained silent because they fear sharing could change others’ perceptions or negatively impact careers. Normalizing mental illness makes it less intimidating and scary for others.
-
RESOURCE
The Power of Personal Stories -- National Alliance on Mental Illness -
PODCASTS
A Hospital CEO opens up about his struggle with panic attacks and anxiety
AHA Podcast Preventing Physician Suicide: A doctor shares his struggle and recovery
-
RESOURCE
- Initiate or enhance your organization’s integration of physical and behavioral health services, or “whole person health.” Research shows that integrated care boosts employee satisfaction, and has a positive return on investment.
-
TOOLS
-
- Consider training your team in Mental Health First Aid. The program has been shown to increase knowledge about mental health, instill greater confidence to assist others in distress, and improve one’s own well-being. MHFA is not the only program, others are listed below.
-
- Lead by example and set the tone for a culture of psychological safety
- Communicate with transparency that the leadership team is committed to eliminating the stigma about psychiatric and substance use disorders.
- • Highlight activities of the team to support a culture of psychological safety and keep the conversation going.
-
-
Assess and address COVID-19 impacts on well-being. Much focus has been on vaccinations, enhanced safety protocols and personal protective equipment to protect the physical health of clinicians and staff, but equally important are resources to protect their mental health.
-
RESOURCE HUBS
Addressing Resilience During COVID-19
Stress and Coping Resources -
AHA REPORT
TrendWatch: The Impacts of the COVID-19 Pandemic on Behavioral Health describes the impacts of the COVID-19 pandemic on behavioral health in the U.S., including looking at the effects on the health care workforce, and innovative ways of providing services. In addition, the report highlights AHA policy recommendations for future actions. -
CASE STUDY
Northwell Health Center for Traumatic Stress, Resilience and Recovery
-
RESOURCE HUBS
-
Assess and address COVID-19 impacts on well-being. Much focus has been on vaccinations, enhanced safety protocols and personal protective equipment to protect the physical health of clinicians and staff, but equally important are resources to protect their mental health.

