

How to Help Clinicians Stay Resilient during COVID-19

The latest COVID-19 surge has led to record levels of hospitalizations and deaths, and health care professionals (HCPs) are suffering heavy casualties as well. The Centers for Disease Control and Prevention reported that as of Dec. 2, more than 247,000 HCPs had contracted COVID-19 and 843 had died from the virus.
 These statistics tell only part of the story of how hospitals and health systems’ front-line caregivers are being adversely affected by the pandemic. Concerns are mounting rapidly about the number of physicians and nurses and other care team members suffering emotionally and physically from treating COVID-19 patients.
These statistics tell only part of the story of how hospitals and health systems’ front-line caregivers are being adversely affected by the pandemic. Concerns are mounting rapidly about the number of physicians and nurses and other care team members suffering emotionally and physically from treating COVID-19 patients.
Many HCPs have seen more death during the pandemic than they’ve seen in their entire careers. They’re physically and emotionally exhausted. They’re worried about their own health and potentially spreading the virus to their loved ones. Many may now need support beyond the wellness services, meals, housing and child care-assistance provided, including access to mental health support. And while addressing the here and now, helping teams find the space and sanctuary to process the immediate impact, many of the efforts hospitals and health systems have undertaken to address burnout also can provide support.
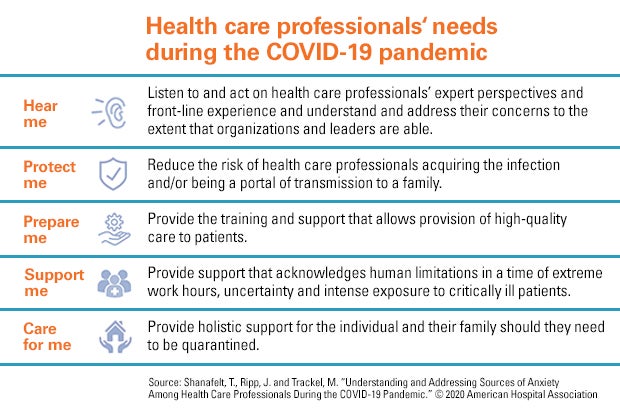
As the AHA’s Well-being Playbook: A Guide for Hospital and Health System Leaders (available to members only) notes, the goal is not simply to create a culture absent of stressors that lead to burnout and fatigue, but to help care teams create a culture of well-being so clinicians can provide the best care for patients and themselves.
4 Places to Start Building Organizational Well-Being
- Create an infrastructure for well-being. Infrastructure must be built to create or expand a culture of well-being. While there are larger efforts underway, there is also a need to celebrate and promote the small wins that support the team.
- Engage your team. The best experts to identify work challenges and the most impactful solutions are those clinicians who work on the front lines; therefore, truly listening is key. Soliciting input provides double the reward as it is both a key process step and a treatment for burnout.
- Implement pilots. Deploy initiatives that are operationalized easily and help build buy-in and momentum for more complex and challenging interventions. Aligning to operational priorities and choosing a willing and engaged group of clinicians to pilot test initiatives will increase success.
- Evaluate impact. Because the causes of COVID-19 fatigue are multifactorial, one intervention may not change the overall exhaustion rate of staff.
Incorporate process metrics like perception of control over workflow, or satisfaction with a particular aspect of clinical care and outcome metrics to evaluate a program‘s success.
Other AHA resources to help your organization address the many stressors of COVID-19 among clinicians include:
Advancing Well-being during and after a Pandemic
In this webinar, Gaurava Agarwal, M.D., assistant professor of psychiatry and behavioral sciences and medical education at the Northwestern Feinberg School of Medicine, shares frameworks that help organizations and individuals understand stress models, manage the causes of pandemic-related anxiety, and identify drivers of burnout.
Measuring the Effectiveness of Burnout Prevention Strategies
In this Advancing Health interview, Read Pierce, M.D., vice president of the AHA’s Physician Alliance and vice president of culture transformation and strategy at the Institute for Healthcare Excellence, and Bryan Sexton, M.D., director of the Duke Center for Healthcare Safety and Quality and associate professor, examine how to measure the work being done to prevent burnout and how to incorporate thriving into the health care culture.



