Medicaid Coverage Supports Rural Patients, Hospitals, and Communities
March 2026
One in seven Americans live in rural areas and rely on rural hospitals and health systems for the health and well-being of their communities.1 The importance of rural hospitals cannot be overstated, as individuals who live in these communities face greater challenges in accessing health care due  to a number of factors, including a lack of affordable coverage options, geographic isolation and a shortage of health care providers.2 Medicaid, which covers 16.1 million people in rural communities, plays a vital role in addressing these barriers and sustaining rural hospitals so they can continue to support patients and their communities.3
to a number of factors, including a lack of affordable coverage options, geographic isolation and a shortage of health care providers.2 Medicaid, which covers 16.1 million people in rural communities, plays a vital role in addressing these barriers and sustaining rural hospitals so they can continue to support patients and their communities.3
Cuts to the Medicaid program, such as those enacted by Congress, will have a devastating impact on rural hospitals and patients.
The Importance of Rural Hospitals
 Rural hospitals serve as critical — and sometimes the sole — source of care for rural communities. Consequently, rural hospitals face elevated levels of uncompensated care that can be linked to higher uninsured rates in rural communities.4 Due to this and other fiscal pressures, many rural hospitals operate under tight margins and face a disproportionate threat of closure.5 About half of rural hospitals consistently experienced negative operating margins from patient services from 2017-2022.6 Some hospitals have dealt with negative margins by reducing costs, which can include eliminating service lines or closing altogether. According to the UNC Cecil G. Sheps Center, over 100 rural hospitals have closed or converted in the last decade.7
Rural hospitals serve as critical — and sometimes the sole — source of care for rural communities. Consequently, rural hospitals face elevated levels of uncompensated care that can be linked to higher uninsured rates in rural communities.4 Due to this and other fiscal pressures, many rural hospitals operate under tight margins and face a disproportionate threat of closure.5 About half of rural hospitals consistently experienced negative operating margins from patient services from 2017-2022.6 Some hospitals have dealt with negative margins by reducing costs, which can include eliminating service lines or closing altogether. According to the UNC Cecil G. Sheps Center, over 100 rural hospitals have closed or converted in the last decade.7
Hospital closures and service line reductions can be devastating to rural communities. Behavioral health and obstetrics care are two examples where despite a significant need for this care in rural areas, providers and services continue to be limited or entirely unavailable in rural communities due to fiscal and other issues.8,9,10 When providers or essential services are not available locally, patients are required to travel long distances or, worse, forego care altogether, leading to health complications and unnecessary hospitalizations.
Medicaid’s Role as a Lifeline for Rural Patients, Communities and Hospitals
There are three primary ways in which Medicaid supports rural communities and hospitals:
1. Medicaid is a critical coverage option for people who live in rural areas.
Medicaid is a significant source of coverage for individuals and families in rural areas who would otherwise not be able to afford insurance. In nearly all states, Medicaid covers a larger share of both adults and children in rural communities than urban communities.11 Nearly 50% of children and 18% of adults in rural communities are covered by Medicaid.12 And nearly 50% of babies born in rural areas are covered by Medicaid.13
2. Medicaid improves access to care in rural areas.
Medicaid is a powerful tool in enabling people to overcome barriers to care. Children with Medicaid coverage are four times more likely to have regular sources of care and two to three times more likely to receive preventive care services than uninsured children.14 Adult Medicaid enrollees are five times more likely to have regular sources of care and four times more likely to receive preventive care services than individuals without coverage. 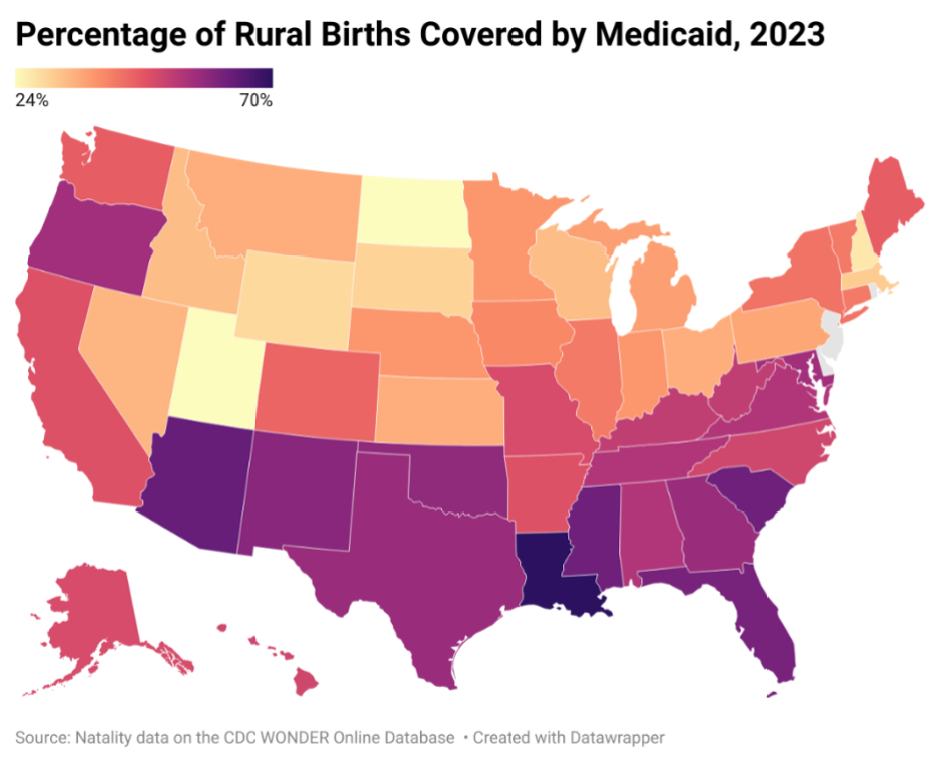 With more patients covered, providers are more likely to be able to sustain themselves financially and, in some cases, expand the services they can offer in rural areas.
With more patients covered, providers are more likely to be able to sustain themselves financially and, in some cases, expand the services they can offer in rural areas.
3. Medicaid stabilizes and strengthens rural hospitals and workers.
Medicaid plays a significant role in reducing uncompensated care and stabilizing hospitals in rural communities. Higher rates of Medicaid coverage for adults have been associated with improved hospital financial performance and lower likelihood of closure, especially in rural areas that have expanded Medicaid. The majority (74%) of rural hospital closures happened in states where Medicaid expansion was not in place or had been in place for less than a year.15
Medicaid coverage directly affects the demand for services in rural areas, and therefore the need for a robust health care workforce. Several studies on the impacts of Medicaid on the primary care and behavioral health workforce showed that states that have expanded Medicaid may be able to recruit, or may attract, additional providers due to the higher demand for services.16
And Medicaid’s contribution to the workforce is not limited to health care providers — rural hospitals typically serve as one of the largest employers in their communities and economic foundations of their local economy. This allows Medicaid to support more economically stable and vibrant communities.
End Notes
- aspe.hhs.gov/sites/default/files/documents/6056484066506a8d4ba3dcd8d9322490/rural-health-rr-30-Oct-24.pdf
- gao.gov/blog/why-health-care-harder-access-rural-america
- kff.org/other/state-indicator/medicaid-enrollees-by-urban-rural-status/?dataView=1¤tTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
- mc.ncbi.nlm.nih.gov/articles/PMC10924546/#:~:text=Rural%20hospitals%20have%20more%20uncompensated,change%20in%20
non%2Dexpansion%20states - kff.org/health-costs/issue-brief/hospital-margins-rebounded-in-2023-but-rural-hospitals-and-those-with-high-medicaid-shares-werestruggling-more-than-others/#:~:text=About%20half%20of%20low%2Dvolume,designation%20had%20negative%20operating%20margins
- aha.org/system/files/media/file/2024/04/Assessing-the-Impact-of-COVID-19-on-Rural-Hospitals-report.pdf
- shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-closures/; converted facilities no longer offer inpatient services but continue to provide some health care services.
- familymedicine.uw.edu/rhrc/publications/changes-in-the-supply-and-rural-urban-distribution-of-selected-behavioral-health-providers/
- gao.gov/products/gao-23-105515
- gao.gov/blog/additional-risks-and-challenges-pregnant-women-rural-and-underserved-communities
- kff.org/medicaid/issue-brief/the-role-of-medicaid-in-rural-america/
- ccf.georgetown.edu/2023/08/17/medicaids-coverage-role-in-small-towns-and-rural-areas/
- aha.org/system/files/media/file/2025/02/Fact-Sheet-Medicaid-20250204.pdf
- ahip.org/resources/the-value-of-medicaid-providing-access-to-care-and-preventive-health-services
- aha.org/system/files/media/file/2022/09/rural-hospital-closures-threaten-access-report.pdf
- EFFECTS OF THE ACA MEDICAID EXPANSION ON THE COMPENSATION OF NEW PRIMARY CARE PHYSICIANS - PMC