Analysis: Hospitals and Health Systems Are Critical to Preserving Access to Care for Rural Communities
Hospitals and health systems play critical roles in preserving access to care for patients in rural America. They have increasingly stepped up to fill voids in access to care by reinvesting through access points like hospital outpatient departments (HOPDs). These sites of care provide essential services for rural and low-income communities. Oftentimes, hospitals have been a lifeline for struggling rural physician practices — helping to keep their doors open. HOPDs, meanwhile, have remained convenient high-quality key points of access for patients with more complex care needs.1
Hospitals Preserve Access to Care for Rural Communities
 The challenging economics of providing care in rural communities contribute to gaps in access. Rural communities, by nature, generally have fewer people and therefore do not generate the health care utilization to finance the full range of health care services. In addition, caring for rural patients can be more costly on a per patient basis as patients in rural communities tend to have more complex health needs, are much more likely to be uninsured, and are more likely to rely on public programs when they do have coverage. It is unsurprising, therefore, that many providers have struggled to stay open and provide care to the patients and community. Hospitals, however, have disproportionately stepped in to support these access points for patients in rural communities. For example, hospitals were two and half times more likely to acquire physician practices in rural areas than other entities, including commercial insurers.2
The challenging economics of providing care in rural communities contribute to gaps in access. Rural communities, by nature, generally have fewer people and therefore do not generate the health care utilization to finance the full range of health care services. In addition, caring for rural patients can be more costly on a per patient basis as patients in rural communities tend to have more complex health needs, are much more likely to be uninsured, and are more likely to rely on public programs when they do have coverage. It is unsurprising, therefore, that many providers have struggled to stay open and provide care to the patients and community. Hospitals, however, have disproportionately stepped in to support these access points for patients in rural communities. For example, hospitals were two and half times more likely to acquire physician practices in rural areas than other entities, including commercial insurers.2
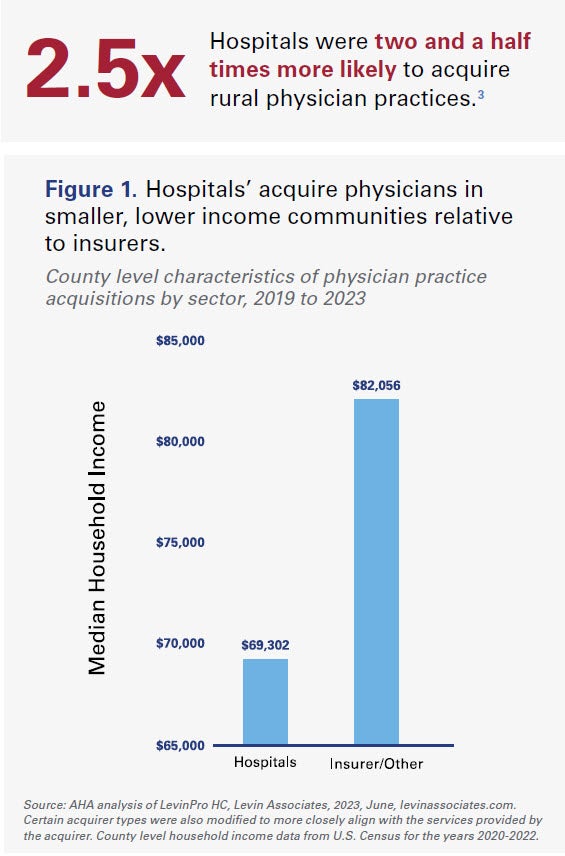
Commercial insurers in particular are overwhelmingly focused on larger, more profitable markets, where the financial upside is greater. Median household income was on average 18.4% higher in counties where insurers acquired physician practices compared to counties where hospitals acquired physician groups (see Figure 1). Additionally, the county level population where commercial insurers acquired physician practices was on average 61.4% larger than it was for hospitals.
Rural Patients Disproportionately Rely on Hospitals to Meet Care Needs
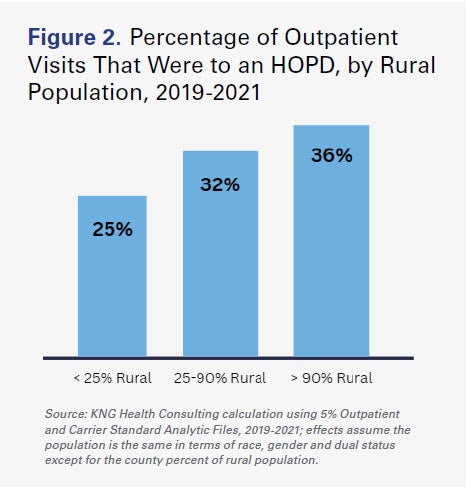 HOPDs are a critical source of care for Medicare beneficiaries in rural areas and for those dually eligible for Medicaid. The more rural the county that a Medicare beneficiary lives in, the more likely their visits take place in an HOPD rather than a physician office.4 For example, for patients from counties where 90% or more of the population lives in a rural area, 36% of physician visits are provided through an HOPD. That number drops to 25% of physician visits for the least rural counties (see Figure 2).
HOPDs are a critical source of care for Medicare beneficiaries in rural areas and for those dually eligible for Medicaid. The more rural the county that a Medicare beneficiary lives in, the more likely their visits take place in an HOPD rather than a physician office.4 For example, for patients from counties where 90% or more of the population lives in a rural area, 36% of physician visits are provided through an HOPD. That number drops to 25% of physician visits for the least rural counties (see Figure 2).
Hospitals Also Disproportionately Care for the Most Vulnerable Patients
Medicare beneficiaries that are dually-eligible for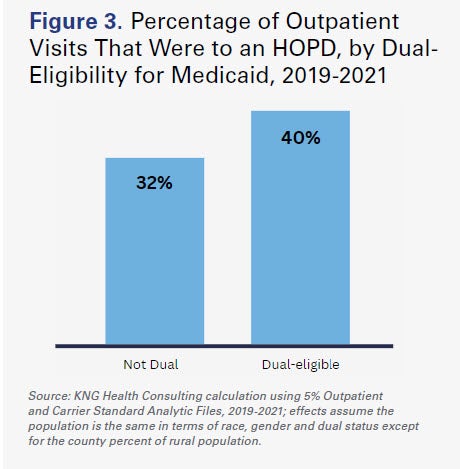 Medicaid also are more reliant upon HOPDs for outpatient care than non-duals, receiving 40% of visits through an HOPD compared to 32% among non-duals (Figure 3). This partially reflects the more complex clinical needs of the dual-eligible population. Among dual-eligible Medicare beneficiaries that received most of their outpatient visits through an HOPD, 72% had a complication or comorbidity (CC), compared to 64% of patients who mostly went to independent physician offices. Further, those HOPD patients had an average of 5.2 CCs, while majority independent physician office cases had an average of 3.6. These trends hold for patients with major complications or comorbidities (MCCs), as well: 38% of majority HOPD cases had an MCC, while 25% of the independent physician office cases did.
Medicaid also are more reliant upon HOPDs for outpatient care than non-duals, receiving 40% of visits through an HOPD compared to 32% among non-duals (Figure 3). This partially reflects the more complex clinical needs of the dual-eligible population. Among dual-eligible Medicare beneficiaries that received most of their outpatient visits through an HOPD, 72% had a complication or comorbidity (CC), compared to 64% of patients who mostly went to independent physician offices. Further, those HOPD patients had an average of 5.2 CCs, while majority independent physician office cases had an average of 3.6. These trends hold for patients with major complications or comorbidities (MCCs), as well: 38% of majority HOPD cases had an MCC, while 25% of the independent physician office cases did.
These facts demonstrate the outsized role of hospitals in preserving 24/7 access to care for the most vulnerable in every community across the nation.
Conclusion
Hospitals and health systems play a key role in ensuring access to care and services for patients across the country. In rural communities, hospitals have increasingly stepped up by reinvesting in HOPDs to maintain care locally for the seniors who rely on it and use it the most. HOPDs provide care for Medicare patients who are more likely to be sicker and more medically complex than those treated at physicians’ offices while also being held to stricter safety and regulatory requirements. This is especially true in rural communities, and additional site-neutral funding cuts being considered by Congress would have a direct impact on the level of care and services available to vulnerable patients in these communities. The AHA continues to urge Congress to reject Medicare payment cuts that would reduce access to essential care and services in communities, especially those in rural and underserved areas.
__________
1 https://www.aha.org/guidesreports/2023-03-27-comparison-medicare-beneficiary-characteristics-report
2 AHA analysis of Levin Associates data on physician medical groups between 2019 and 2023.
3 Compared to other entities, including commercial insurers, private equity, and other entities, excluding the acquisition of physician practices
by other physician practices.
4 KNG Health Consulting calculation using 5% Outpatient and Carrier Standard Analytic Files, 2019-2021.