

Studies: Telemedicine Pays Dividends in Rural Health

Deploying telehealth in rural areas and elsewhere to deliver care more efficiently while reducing costs and expanding access continues to accelerate. And the evidence is mounting that virtual care is delivering on these promises.
This was a hot topic at the recent AHA Rural Health Care Leadership Conference, where rural hospital and health system leaders shared strategies and information about how they’ve expanded telehealth services to areas like behavioral health emergency assessments, obstetrics, nephrology and neurology.
Yet, for all the progress being made to leverage technology and clinical expertise to bring care more efficiently to those in rural and remote areas, detailed studies on the clinical and financial impact of these efforts have been few and far between. But this, too, is changing.
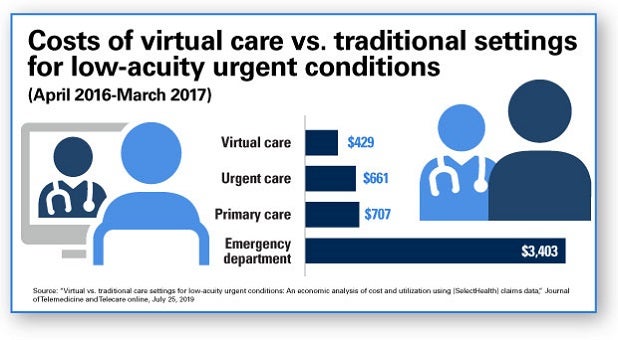
A study conducted by Intermountain Healthcare leaders and published in the Journal of Telemedicine and Telecare showed that the total cost for some of the most common virtual diagnoses was sharply lower than in other care settings. The study, which looked at SelectHealth (a nonprofit health plan serving 900,000 members in Utah, Idaho and Nevada) claims between April 2016 and March 2017, reported that the $429 total cost of virtual care for the most common telehealth diagnoses was $232 less than urgent care, $278 less than primary care and $2,974 less than diagnoses delivered in the emergency department.
Intermountain’s Connect Care Pro 24/7 on-demand telehealth system provides services in seven western states and to many facilities that are not part of Intermountain, which began offering neonatal telehealth services in 2012. Marc Harrison, M.D., Intermountain Healthcare’s president and CEO, noted in the Harvard Business Review that telehealth has had a profound impact on patients and the health system.
Aside from driving significant decreases in unnecessary ED and urgent care utilization, Intermountain Connect Care Pro has contributed to decreased mortality and intensive care unit lengths of stay, improved door-to-door time for stroke patients, and decreased evaluation time for behavioral health patients in crisis. The program also has had a significant impact on preventing unnecessary and costly patient transfers for newborn and ICU patients.
Another more recent telehealth study, albeit much smaller in scope, conducted by the Mayo Clinic found that using an asynchronous telehealth platform for consults with infectious disease experts resulted in a sharp reduction in risk of death within 30 days, as well as a decreased risk of rehospitalization. The study at Mayo Clinic’s Albert Lea and Austin hospitals in southeastern Minnesota, saw a 70% reduced risk of death within 30 days and a trend toward reduced readmission within 30 days.
5 Ways Telehealth Is Benefiting Patients, Providers and Payers
Many factors are driving the growth of telehealth services in rural areas, from changing demographics and consumerism to a continuing shortage of providers to advancing technology.
As these studies demonstrate, provider organizations, patients and payers are seeing the following benefits:
- Enhanced access to care.
- Improved patient convenience.
- High degree of provider satisfaction.
- Increased levels of sustainable services.
- Reduced cost of staff and patient travel.
Visit the AHA's Small or Rural Hospitals page for more Rural Health resources.



