Fact Sheet: Telehealth
April 2025
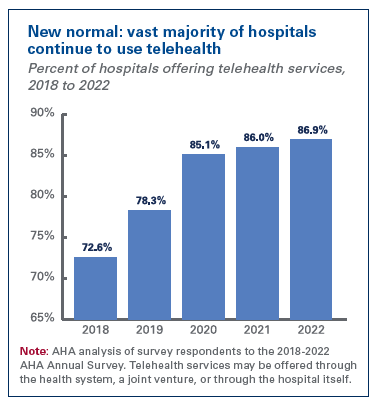 Telehealth is now a routine way for patients to access health care services and for providers in remote and other areas to access specialty consults that expand their ability to treat patients in their local communities. Telehealth adoption has grown significantly over the past five years due to waivers that enabled more services to be delivered via telehealth under more circumstances and for the providers of those services to be reimbursed. It has been proven safe and effective, and both patients and clinicians report high satisfaction. Prior concerns that telehealth would add utilization — and therefore cost — to the health care system have not been borne out.
Telehealth is now a routine way for patients to access health care services and for providers in remote and other areas to access specialty consults that expand their ability to treat patients in their local communities. Telehealth adoption has grown significantly over the past five years due to waivers that enabled more services to be delivered via telehealth under more circumstances and for the providers of those services to be reimbursed. It has been proven safe and effective, and both patients and clinicians report high satisfaction. Prior concerns that telehealth would add utilization — and therefore cost — to the health care system have not been borne out.
Unfortunately, without congressional action, patients and providers may soon lose access to important telehealth services. We urge Congress to not send the health care system backward and instead make permanent the telehealth flexibilities granted during the pandemic.
AHA Position
As outlined in our telehealth advocacy agenda, the AHA supports:
- Permanently adopting expanded access to telehealth: Permanent adoption of telehealth flexibilities will provide a firm foundation to preserve access and support further reform. We urge Congress to lift geographic and originating site restrictions, allow Rural Health Clinics and Federally Qualified Health Centers to serve as distant sites, expand practitioners who can provide telehealth, remove arbitrary in-person visit requirements for behavioral health, and allow the continuation of audio-only telehealth services.
- Expanding the telehealth workforce: Expanding the telehealth workforce will serve as a force multiplier to increase access for areas with health care staffing shortages. Specific policies (like codifying virtual supervision flexibilities), removing barriers to cross-state licensure and eliminating dangerous reporting requirements (like provider home addresses) will increase the telehealth workforce.
- Ensuring fair and adequate telehealth reimbursement: Virtual care still has costs, including for both personnel, technology, and office space out of which many telehealth providers work. Appropriate reimbursement is necessary to preserve increased access to care.
- Supporting telehealth for rural and medically underserved areas: One barrier to expanding telehealth to these populations has been a lack of access to enabling technologies (like broadband, reliable Wi-Fi or smartphones), as well as education to support digital literacy. As such, we encourage cross-agency collaboration to develop training and infrastructure investment. Additionally, arbitrary requirements, like mandatory in-person visit requirements for behavioral health or prior to prescribing of controlled substances, have limited access for communities that may not have a practitioner available in person. We have urged for the development of a new, streamlined special registration process to waive in-person visit requirements for prescribing controlled substances.
Key Facts
- Recent data from the Kaiser Family Foundation indicates that while utilization of telehealth has declined since 2020, utilization remains higher than pre-pandemic levels. In the last quarter of 2023, over 12.6% of Medicare beneficiaries received a telehealth service.1
- There is a growing body of evidence showing that telehealth does not result in additive or duplicative care. A study of over 35 million records by Epic found that for most telehealth visits across 33 specialties, there was no need for an in-person follow-up visit within 90 days of the telehealth visit.2
- Recent data suggest that the United States will face a physician shortage of up to 86,000 physicians by 2036.3 Telehealth is a critical supporting element to address the growing shortage of physicians.
- Patients across geographies and settings, including both rural and urban areas, have benefited from the increased access and improved convenience provided by telehealth services since patients could receive care from their homes. In fact, data from the Office of the Assistant Secretary for Planning and Evaluation (ASPE) showed that most patients using telehealth in 2020 (92%) received telehealth from their home.4 >/li>
- The availability of audio-only telehealth is a critical option to ensure access to care when patients may not have access to technology or bandwidth for video visits. A 2021 report from ASPE found that the majority of surveyed respondents 65 and older used audio-only visits (56.5%) compared to video visits, partly driven by the fact that over 26% of Medicare beneficiaries reported not having computer or smartphone access at home.5
- The lack of broadband infrastructure exacerbates access challenges for certain areas. The Federal Communications Commission reports that over 22% of Americans in rural areas lack access to appropriate broadband (fixed terrestrial 25/3 Mbps) compared to 1.5% in urban areas.6
- Misperceptions about telehealth contributing to fraud, waste and abuse are not supported by data. A recent Office of the Inspector General report found that only 0.2% of all telehealth providers were “potentially high-risk” for fraud, waste and abuse previously.7 Policies should support the 99.8% of providers safely and compliantly delivering services.
Resources
- Taking Action to Extend Telehealth and Hospital-at-home Programs
- CMS Urged to Remove Telehealth Provider Home Address Reporting Requirements
- AHA Comments on CMS’s Physician Fee Schedule Proposed Rule for Calendar Year 2024
- AHA urges Congress to make telehealth flexibilities permanent
- AHA Comments on 340B Drug Pricing Program, IRF Payments, Physician Fee Schedule and Telehealth
- AHA Letter of Support for Senate CONNECT Health Act of 2023 (S. 2016)
- AHA’s Feedback to the Senate Re: The CONNECT Act
- AHA Comments on the SUPPORT for Patients and Communities Reauthorization Act
- AHA Letter to DEA Regarding Request for Release of Special Registration for Telemedicine Regulation
Notes
- https://www.kff.org/medicare/issue-brief/what-to-know-about-medicare-coverage-of-telehealth/
- https://epicresearch.org/articles/telehealth-visits-unlikely-to-require-in-person-follow-up-within-90-days
- https://www.aamc.org/media/75236/download?attachment
- https://aspe.hhs.gov/sites/default/files/documents/a1d5d810fe3433e18b192be42dbf2351/medicare-telehealth-report.pdf
- https://aspe.hhs.gov/sites/default/files/documents/4e1853c0b4885112b2994680a58af9ed/telehealth-hps-ib.pdf
- https://www.fcc.gov/reports-research/reports/broadband-progress-reports/2020-broadband-deployment-report
- https://oig.hhs.gov/oei/reports/OEI-02-20-00720.pdf