Improving Quality and Patient Safety
The Members in Action series highlights how hospitals and health systems are implementing new value-based strategies to improve health care affordability. This includes the work described below to improve quality and outcomes.
 | Presbyterian Healthcare Services – Albuquerque, NM Presbyterian Healthcare Services found that treating patients at home helps prevent the onset of delirium, reduces fall risk, reduces the risk of infection and allows for increased mobility. Their Hospital at Home program bolstered the hospital’s response to COVID-19 by enabling PHS to triple their capacity for at-home admissions and free up hospital beds for patients that needed them most. Read more.
|
Mount Sinai Health System – New York, N.Y. Because of their existing Hospitalization at Home program, Mount Sinai was able to quickly start a new program, Completing Hospitalization at Home, to focus on non-COVID-19 patients and expanded to include low- to medium-acuity COVID-19 patients once adequate personal protective equipment was available. Read more.
|
 | Children’s Wisconsin – Milwaukee, Wisconsin By expanding communication with patients and families throughout the continuum of care, Children’s Wisconsin sees a higher engagement of family caregivers in their children’s health, leading to fewer visits to the ED and a decrease in avoidable readmissions. Improved communication among providers also yielded a reduction in clinical variation. Read more.
|
 | Parkland Health & Hospital System – Dallas, Texas Parkland Hospital & Health System uses social determinants of health data to guide its prevention and clinical efforts to reduce incidents of breast cancer. For example, data from its’ EHR, a cancer registry and its community health needs assessments led the system to revamp its outreach campaigns to target neighborhoods where patients with the most need live. Parkland also provides information to case managers and clinicians on which patients may need food pantry vouchers, housing referrals or transportation assistance to supplement clinical and pharmacological interventions. Read more here. |
 | Grady Health System – Atlanta, Ga. Grady Health System uses artificial intelligence and predictive analytics to provide proactive care management for patients with diabetes and chronic heart failure. By utilizing data from electronic health records, Grady stratifies inpatients into risk categories to direct assistance to those most in need of support, and reduce avoidable readmissions and preventable ED visits. Click here to read more. |
 | Adventist Health Castle – Kailua, Hawaii Adventist Health Castle’s Empathy In Action program is a research-based curriculum that teaches staff and volunteers listening skills and demonstrates empathetic approaches to engaging with patients, families and colleagues. Castle credits the program for improving patient satisfaction and employee engagement scores. Click here to read more. |
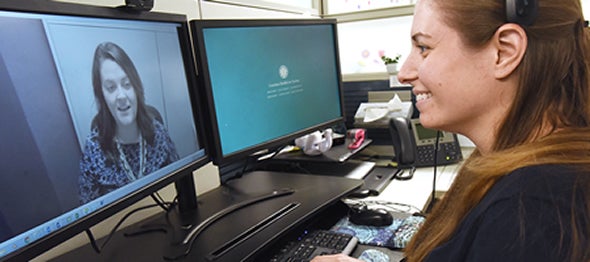 | Atrium Health – Charlotte, N.C. To increase access to behavioral health care, Atrium Health employs a virtual behavioral health integration program at 36 of its primary care and pediatric sites. The team-based model uses virtual platforms to improve timely access to behavioral health services, lower the overall cost of care and improve the patient experience. Click here to read more. |
 | Presbyterian Healthcare Services – Albuquerque, NM Presbyterian Healthcare Services’ statewide-partnership, called The Substance Use Disorder and Community Collaborative Initiative, delivers compassionate, high-quality, evidence-based care for patients with substance use disorder. Changing the culture of treating patients with SUD as any other chronic condition, devoid of judgment, is a key element of the approach. Click here to read more. |
 | Montefiore Health System – The Bronx, Westchester and the Hudson Valley, N.Y. Montefiore Health System uses the Collaborative Care Model to better serve patients with significant medical and mental health conditions and socioeconomic challenges. By leveraging digital tools, such as a smartphone, Montefiore can improve outcomes and facilitate better communications with providers. Click here to read more. |
 | Geisinger Health System – Danville, PA In 2015, Geisinger Health System piloted a patient refund program to encourage criticism, inviting patients to alert staff of areas they could improve. A year later, the program expanded to all 10 of the system’s hospitals. The effort is part ofGeisinger’s ProvenExperience® program, which includes other initiatives, such as leadership rounding, uniform standards and respectful interactions with patients and families. Click here to read more. |
 | Birmingham VA Medical Center – Birmingham, AL Birmingham VA Medical Center’s “Whole Health Approach to Opioid Safety,” revolves around weekly, 90-minute shared medical appointments that address opioid reliance among the medical center’s veteran population. Click here to read more.
|
 | Ochsner Health System – Jefferson, LA Ochsner Health System is breaking new ground by implementing an early-warning system aided by artificial intelligence designed to proactively prompt clinicians to intervene in a patient’s care. In a 90-day pilot, the warning system helped reduce adverse events outside of the intensive care unit by 44 percent, a rate officials believe will increase over time. Click here to read more.
|
 | Augusta Health – Fishersville, VA Augusta Health dramatically improved patient outcomes and reduced readmissions with its own automated sepsis surveillance system. When a patient’s condition triggers an alert, a secure text is sent to the ED charge nurse for immediate assessment. Click here to learn more. Click here to read more. |
 | Parkland Health & Hospital System – Dallas, TX Parkland Health & Hospital System, launched a program that allows certain patients, rather than medical professionals, to self-administer long-term antibiotics. This has allowed Parkland to maximize limited resources and eliminate inpatient stays for patients that could be treated at home. Click here to read more. |
 | Rush University Medical Center – Chicago, IL Rush University Medical Center uses an app to support its enhanced recovery after surgery program and sees reduced hospitals stays. Click here to read more. |

